Syndesmosis sprains : The high ankle injury
You may have heard various athletes suffering a high ankle sprain or injuring their syndesmosis. But what exactly is a syndesmosis injury? And how does it differ to a normal lateral ankle sprain?
The ankle syndesmosis is the joint between the distal (lowest aspect) of your tibia and fibula. It is comprised by three main supporting ligamentous structures – The Anterior inferior tibiofibular ligament, Posterior inferior Tibiofibular ligament, and interosseous membrane (see Figure 1). The role of the syndesmosis is to provide stability to the tibia and fibula and resist separation of these two bones during weightbearing tasks. It also plays a role in assisting with mobility of the ankle.
You may have heard various athletes suffering a high ankle sprain or injuring their syndesmosis. But what exactly is a syndesmosis injury? And how does it differ to a normal lateral ankle sprain?
The ankle syndesmosis is the joint between the distal (lowest aspect) of your tibia and fibula. It is comprised by three main supporting ligamentous structures – The anterior inferior tibiofibular ligament, posterior inferior tibiofibular ligament, and interosseous membrane (see Figure 1). The role of the syndesmosis is to provide stability to the tibia and fibula and resist separation of these two bones during weightbearing tasks. It also plays a role in assisting with mobility of the ankle.
How does it differ to a common ankle sprain?
Generally, a lateral ankle sprain is a result of and inversion injury and will result in an injury to the outside ligaments of your ankle (ATFL, CFL, PTFL). These ligaments are positioned slightly lower than the syndesmosis and provide stability to the true ankle joint.
Mechanisms of injury:
The most common mechanism for injuring your syndesmosis is a forced dorsiflexion combined with an Eversion movement. Essentially the foot/ankle moves in an upward direction and to the outside of the leg (See figure 3).
The syndesmosis can also be injured with a typical inversion or lateral ankle sprain (Figure 2) mechanism. This usually occurs when the incident is of high force and will result with an injury to the lateral ligaments as well.
Signs and symptoms:
· Mechanism of injury consistent with a syndesmosis injury (forced dorsiflexion + Eversion)
· Pain location may extend above the ankle and into the lower shin
· Swelling may sit slightly above the cease line of the ankle joint
· Difficulty weightbearing, particularly when the foot is in dorsiflexion (knee over toe)
· Low confidence/feeling of instability
Gradings:
Grade 1: isolated injury to the AITFL
Grade 2: Injury to the AITFL and interosseous membrane
Grade 3: Injury to the AITFL, interosseous membrane and PITFL
Grade 4: Injury to the AITFL, interosseous membrane, PITFL and deltoid ligament
Immediate management:
As always if you have recently suffered an injury, please seek medical attention from your physio or doctor for accurate diagnosis and management.
If a syndesmosis injury is suspected acute management will initially involve offloading and protecting the tissues. This may be in the form of one or a combination of crutches, a cam walker (moon) boot and strapping.
Your physio or Doctor may also refer you for imaging such as an x-ray or MRI to assist with diagnosis and understanding the severity of the injury.
Following the acute period of offloading and protection a period of rehabilitation will be required to restore normal function of the foot and ankle. In more severe cases surgery may be required to stabilise the syndesmosis and therefore rehab will commence following a period of protection post-surgery.
If you have experienced an ankle sprain yourself, please book in with one of our physiotherapists for an individualised rehabiltation program.
Relative Energy Deficiency in Sport (RED-S)
Are you unable to recover between training sessions? Experiencing severe wide-spread muscle ache/DOMS? As a female athlete, has your menstruation ever been affected by your training? These can all be signs of energy deficiency and overtraining. Our blog explores what energy deficiency is, how to identify it and how to treat it.
Are you unable to recover between training sessions? Experiencing severe wide-spread muscle ache/DOMS? As a female athlete, has your menstruation ever been affected by your training? These can all be signs of energy deficiencies and overtraining. Our blog explores what energy deficiency is, how to identify it and how to treat it.
What is RED-S?
Relative Energy Deficiency in Sport (or RED-S) is due to low energy availability in athletes. This means the fuel going into the body from food is less than the energy burnt during exercise. This energy balance should be at least equal and is additional to the normal calories consumed during the day. When energy input is at a deficit, RED-S can have significant impact on many body systems, affecting both injury risk and performance.
RED-S used to be known as the ‘female athlete triad,’ terminology which is no longer used as it affects ALL athletes. The most well-known consequences of poor energy availability are bone stress injury and female athletes losing their period. These are both extreme consequences of RED-S, however there are much earlier signs and symptoms which are lesser known.
Signs and Symptoms
· Poor sporting performance
· Inability to recovery between sessions
· Poor wound healing
· Regular cold and flu sickness
· Irregular/cessation of menstruation/periods (see below; ‘The female athlete’)
· Poor bone health/osteopenia/bone stress response
· Mood changes
· Iron deficiency
· Arrythmias (in severe cases)
Why does it matter?
1. Adverse effect on performance
· Quicker onset of fatigue from less energy available to skeletal muscles
· Reduction in muscle strength/size due to impaired testosterone production and compromised neuromuscular control
· Impaired recovery increasing the risk of overtraining
2. Impact on health and wellbeing
· Increased the risk of chronic fatigue
· Low energy availability decreases the ability to heal from injury. Strains, sprains, cuts and bone injuries will take longer to heal
· Impaired growth and development from inadequate cell turnover
The good news is most effects of RED-S are reversible if picked up early.
Athletes are often worried increasing food intake can result in weight gain. This is not the case for most athletes. Nutritionists and sports science professionals understand the energy demands of sport and ensure the balance between energy input and output is correct.
The female athlete
1. Menstruation
If an athlete has low energy availability, their body is unable to produce normal levels of hormones. This can affect the menstrual cycle in female athletes. Periods may become irregular, or even cease altogether. Although the female menstrual cycle is variable between individuals, an individual’s cycle should be quite consistent. Irregularity or cessation of periods for longer than 6 months, or not getting a period by 16 years of age should be reviewed by a doctor.
2. Contraception
Female athletes may be advised the oral contraceptive pill can treat symptoms and normalise their menstrual cycle. The combined pill produces a synthetic estrogen the body can not process and therefore does not assist with improving bone health. This can mask hormonal problems, without assisting in bone health. Athletes using contraception that contains estrogen may also be screened for risk factors of RED-S. Athletes using contraception that alters the normal production of a period (e.g. Mirena, Implanon) must also be monitored for RED-S symptoms.
How can physio help?
Physios can help review your training program and lifestyle to assess energy availability. If an athlete is at significant risk of RED-S, a Sports Physician should be involved to identify any hormonal/nutritional deficiencies and directly address them. This is commonly done through a blood test.
After any nutritional deficits have been addressed, a physio can help modify training loads and aid with recovery techniques.
Who else can help?
Sports doctor – Vital for initial diagnosis and hormonal/nutritional testing. Depending on severity, medical intervention may be needed (e.g. iron infusion)
Nutritionist – Eat the right food… and enough food, is vital for good energy availability
Strength and conditioning coach – Clever programming results in efficient training and decreases the risk of overtraining.
Low Back Pain Myths
There is a lot of information out there on low back pain and injuries. Some of which is very useful but on the other hand there is a lot of misinformation which can sometimes lead us in the wrong direction. In this blog we will look to debunk some of the most common low back pain myths!
There is a lot of information out there on low back pain and injuries. Some of which is very useful but on the other hand there is a lot of misinformation which can sometimes lead us in the wrong direction. In this blog we will look to debunk some of the most common low back pain myths!
Myth # 1 : I Should brace my core or I will get pain
This is a very common thought and is a big reason why people seek help for their low back. Although we have previously thought bracing can help relieve symptoms it can in fact increase the forces going through the back and in some cases lead to pain. The muscles around the trunk play an import role in movement and stability but trying to actively brace these muscles can often lead to stiffness and inefficient movements. The body is clever, our trunk muscles will naturally contract and work when required to assist in tasks such as lifting.
Myth # 2: My low back pain is cause by my back/pelvis being out
One of the most common myths when it comes to low back pain. The back is extremely strong and robust and without serious trauma or force the back and pelvis does not go ‘out’. Manual therapy techniques such as manipulations and adjustments DO NOT put these structures back in to place but they can however provide pain relief which is helpful in the short term.
Myth # 3: I have a disc bulge and degeneration and that is causing my pain
Disc bulges and degeneration are very common and have a high occurrence rate amongst people who don’t have low back pain. We consider these changes to be age related and are not necessarily linked to pain. Approximately 30% of people in their 20’s will have a disc bulge in the absence of low back pain and this percentage goes up approximately 10% for every decade in life. Further to that disc bulges and protrusions have shown to recover on imaging over time. So, it is likely that a disc bulge that you may have previously had is no longer there!
Myth # 4 I need to stand and sit in “good” posture, or I will get pain
There is no such thing as good or correct posture! Despite what we have previously thought and what we may have been told as kids. Research has showed us that there is no direct link to how we sit and stand and pain. Instead, it is recommended to find a posture that you are comfortable with. This may differ from person to person but that is okay. Of course, it is always recommended to keep moving, so taking regular breaks to move around may help reduce the occurrence of discomfort from prolonged positions.
Myth # 5 Bending your back when lifting is bad for your back and you should lift with my knees
The spine holds some very important structures, and it would be a big design flaw if the back was not robust and strong to protect them. In fact, it is one of the strongest parts of the body and can handle large forces. When trained correctly the spine can comfortably handle loads in positions of lifting, squatting and twisting. We are often told to avoid bending the back when lifting however this can often create problems such as inefficient movements and fear avoidance. Like all activities, we need to exposure our body to them for us to get better at it!
Our physiotherapists at East Vic Park Physiotherapy can help answer all your low back related questions. If you would like more information or help with your low back do not hesitate to get in touch!
Costochondritis - A real pain in the chest
There can be many medical reasons for chest, rib and upper back pain including heart and lung conditions, infections and trauma incidences like fractures.
However, once that has been ruled out a diagnosis to be considered is costochondritis.
The condition is classified as inflammation of the costochondral junction of the ribs (where the bone and cartilage meet) or of the costosternal joints (where the ribs connect to the chest bone). The issue is normally unilateral (one sided) but can sometimes be bilateral.
There can be many medical reasons for chest, rib and upper back pain including heart and lung conditions, infections and trauma incidences like fractures.
However, once that has been ruled out a diagnosis to be considered is costochondritis.
What?
The condition is classified as inflammation of the costochondral junction of the ribs (where the bone and cartilage meet) or of the costosternal joints (where the ribs connect to the chest bone). The issue is normally unilateral (one sided) but can sometimes be bilateral.
Signs and symptoms:
- Chest pain that can radiate into the upper chest near the shoulder, down the rib into the area under the armpit and even into the back near your shoulder blade
- Pain can be sharp with certain movements and a dull ache at rest
- Sometimes there is visible swelling over rib joints
- Neck and shoulder range can be affected
- Pain with laughing, coughing, sneezing and deep breathing
Why?
The exact reason for an individual developing inflammation of that particular area is yet to be determined. However, there are a few mechanisms that have been anecdotally found to trigger costochondritis symptoms including:
- Trauma to the area (eg. Direct fall/pressure or injury to the pec muscle)
- Intense exercise of the area
- A bout of illness with lots of coughing
Diagnosis methods
The condition is primarily diagnosed with clinical tests including:
- Palpation of the costochondral and costosternal joints (usually ribs 2-5)
- Assessment of thoracic, cervical and glenohumeral joint range
- Cough/sneeze/laugh test
- Deep breathing test
Scans would only be beneficial if you needed to rule out any of the below alternate diagnoses. Potentially a blood test would be beneficial if a multi joint inflammatory condition is suspected.
Examples of differential diagnosis
- Coronary artery disease (or other heart conditions acute or chronic)
- Pulmonary embolism or pneumothorax
- Rib fractures or subluxations
- Costovertebral sprain
- Tietze syndrome
- Pectoralis muscle injury
- Infections (e.g., pneumonia)
- Xiphoidalgia
Treatment
- A review with a physiotherapist can be helpful to accurately diagnose
- Ice over the joints or heat over the muscles
- Speak to your pharmacist regarding pain relieving medication
- Modification of aggravating activities
- Gentle massage to the neck, shoulder and chest muscles can be helpful in some cases
- Gentle stretches and strengthening exercises once the pain has reduced
If you believe you are suffering from costochondritis then book an appointment to see one of our friendly physiotherapists today!
Knee osteoarthritis: is it as debilitating as we think?
Osteoarthritis (OA) is the result of wear and tear of the joint cartilage. It can result in pain and stiffness when loading a joint. But is OA always a sign we need to protect our joints and stop certain activities? The answer may surprise you.
Osteoarthritis (OA) is the result of wear and tear of the joint cartilage. It can result in pain and stiffness when loading a joint. But is OA always a sign we need to protect our joints and stop certain activities? The answer may surprise you.
What is OA?
Osteoarthritis is a break-down of the cartilage in our joints. It mostly affects weightbearing joints such as hips and knees and these joints are subject to larger forces. It was previously thought that joints with OA were to be ‘protected’ by limiting how much we bend, move and load them. We now know this is not true – in fact exercise is one of the most effective ways of reducing osteoarthritic pain.
Knees in particular appear to have many connotations around them and it is widely (but incorrectly) thought that exercise is harmful to our knees. In fact it is quite the opposite – weight bearing exercise helps bone, muscles and other soft tissue adapt to make our knees stronger and more robust. This means an improvement in joint range of motion, muscle length and strength and functional capacity.
How much value should you place on a scan?
It is also important to know that while a scan may show significant osteoarthritic findings, this certainly does not correlate to pain, function or quality of life! Even with ‘severe’ osteoarthritic findings on a scan, very positive functional outcomes can be seen with the above program.
What will help?
The latest guidelines around osteoarthritis, show the most effective way to slow the progression of the pathology is to perform regular weight bearing, strength based exercise. There is good evidence to say this can also significantly reduce pain and improve function. Anti-inflammatories may also help pain and swelling, however you should always consult your doctor before using medication.
It is recommended to perform land based strength exercises 2-3x weekly, such as squats, steps up or leg press. The sets, reps and weight will initially be determined by strength, function and pain levels. This is nicely complimented by aerobic exercises such as walking, bike riding or pool based exercise, although aerobic exercise is not shown to have the same benefit as land-based strengthening.
Our physiotherapists can create a knee strengthening program you can perform at home, all tailored to your individual goals and ability.
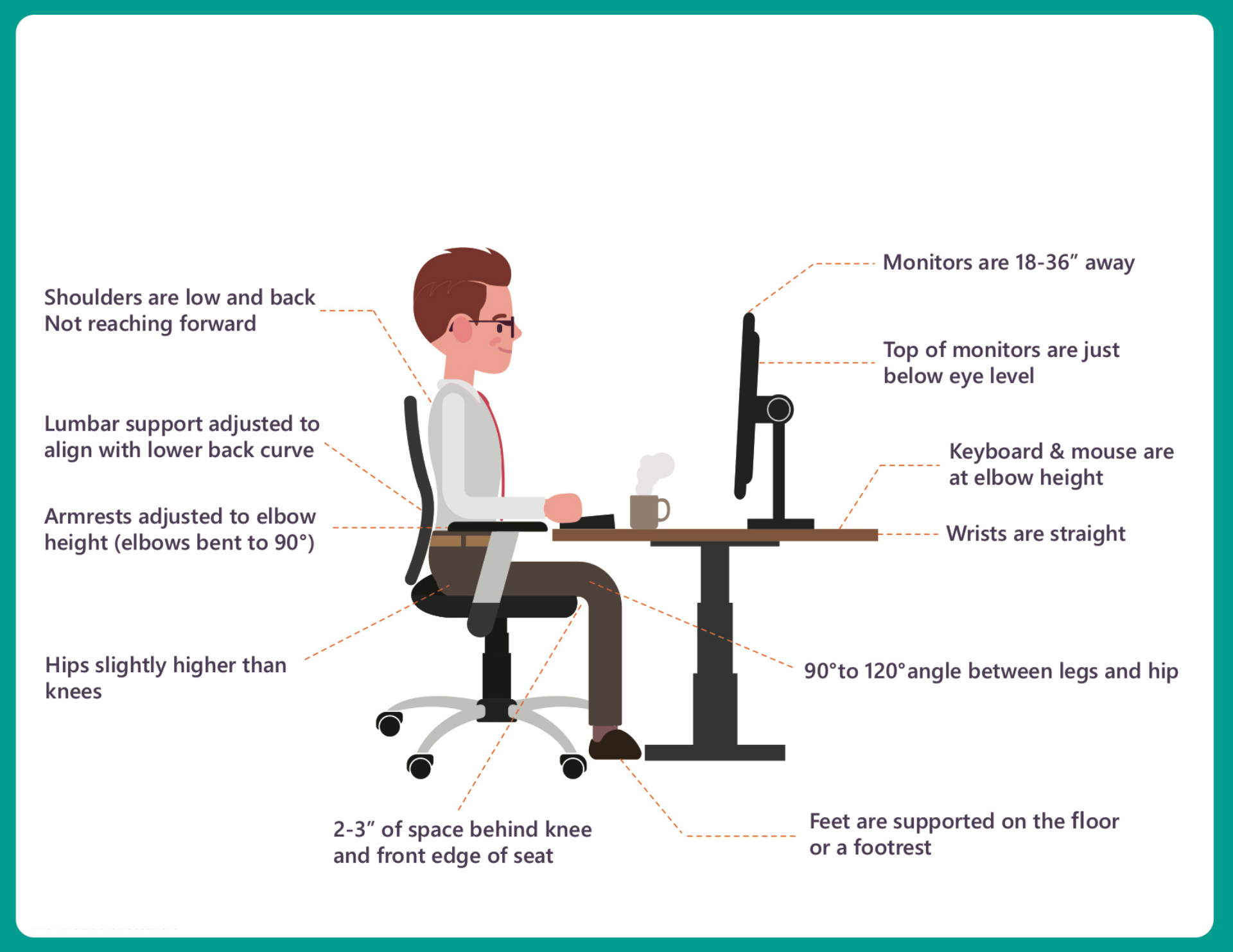
Workstation Ergonomics: Tips to staying pain free
With a large percentage of people now working from home the team at East Vic Park Physio thought it would be a good idea to provide some simple but useful information on workstation ergonomics.
Previous to what we used to think, there is not one way to correctly sit at your workstation. Your set up should be able to accommodate for a range of comfortable positions that you can frequently change throughout the day.
With a large percentage of people now working from home the team at East Vic Park Physio thought it would be a good idea to provide some simple but useful information on workstation ergonomics.
Previous to what we used to think, there is not one way to correctly sit at your workstation. Your set up should be able to accommodate for a range of comfortable positions that you can frequently change throughout the day. The optimal/most comfortable sitting position will change from person to person and will depend on:
The type of work being done
Visual demands
Individual body shape
Figure 1: An example of an acceptable sitting position. It will allow for a range of supported postures that can be changed throughout the day.
Tips for setting up your home workstation:
Sitting with body close to desk
The head and neck are in a forward facing and in midline position (i.e no backward arching of the neck and or forward extension of the chin)
The shoulders are relaxed and relatively symmetrical, elbows close to the side of the body
The back is supported by the chair backrest. The curved lower part of the backrest should sit into the lower back
Having an open angle of 100-120 degrees (slightly more than right angles) at the hip. This can be achieved by adjusting the seat pan tilt and the backrest
o As a general rule have your knees at a height lower than your hip
Ensuring a gap or 2-3 fingers widths between the front of the chair and the back of your knees
Having feet flat on the floor or footrest
Compartment Syndrome: The muscle pain not to be missed!
Earlier this year, St Kilda football club’s caption, Jarryn Geary, sustained an innocuous quad corkie, which later developed into compartment syndrome requiring immediate emergency surgery. Compartment syndrome is a serious condition which can occur acutely or over time and often requires prompt medical attention. Do you know the signs and symptoms to look out for?
Compartment Syndrome is a condition where excessive pressure in a muscle compartment restricts blood supply to that muscle. Muscles are surrounded by fascial connective tissue, which has very poor elasticity. Excessive swelling in the fascial compartment results in compression of blood vessels, then resulting in a reduction of oxygen to that muscle.
Causes
Compartment Syndrome can occur acutely after a traumatic injury (eg fracture, contusion or surgery), or as the result of a blood clot. This is caused by ongoing swelling or bleeding entrapped in the muscle’s fascial casing, increasing pressure within the muscle compartment.
Occasionally compartment syndrome can have no apparent cause, and develops over weeks or months, triggered by vigorous exercise such as running or cycling. Symptoms of chronic compartment syndrome typically worsen throughout exercise and ease with rest.
Signs and Symptoms:
- Severe pain in the muscle
- Swelling or tightness
- Pale or waxy appearance of the skin (due to restricted blood supply)
- Pins and needles, burning or numbness
What do I do if I suspect compartment syndrome?
Get assessed as soon as possible by your physio or GP, particularly if you have a history of trauma to the area. Through careful assessment, your health professional will determine if compartment syndrome is likely, and will refer you on as necessary.
Acute compartment syndrome is considered a medical emergency and can be life threatening if not addressed promptly. Insufficient blood supply over a long period of time means the area is deprived of oxygen and can result in tissue and nerve necrosis (death).
Chronic compartment syndrome can be harder to diagnose, due to transient symptoms that ease with rest. A measurement of intracompartmental pressure can be used to determine the severity of swelling in the fascial compartment. A pressure higher than 30mmHg indicates excessive pressure in the compartment. A CT or MRI scan may be recommended to rule out other serious pathologies.
Treatment Options
Acute compartment syndrome is a medical emergency and a fasciotomy of the affected compartment must be performed immediately to prevent permanent tissue damage. This involves cutting the encasing fascia of the muscle to release pressure, decompress the blood vessels and restore blood flow to the area.
In chronic compartment syndrome, it is recommended trying conservative rehabilitation, firstly by reducing or ceasing physical exercise/activities that exacerbate symptoms. From there, a physiotherapist can assess your strength and biomechanics, to identify any factors that may influence the condition. A referral to a sports doctor may be appropriate to discuss medication options. If conservative rehabilitation fails, or if an individual would like to continue their sport at the same level of intensity, fasciotomy surgery needs to be considered.
Thoracic Outlet Syndrome - A different shoulder diagnosis
The ‘Thoracic Outlet’ describes the compression of nerves (brachial plexus), arteries and veins resulting in pain, and altered sensations in and around the neck, chest and shoulder area. This is a rare syndrome only affecting 8% of the population.
What is thoracic outlet syndrome (TOS)?
The ‘Thoracic Outlet’ describes the compression of nerves (brachial plexus), arteries and veins resulting in pain, and altered sensations in and around the neck, chest and shoulder area. This is a rare syndrome only affecting 8% of the population.
There are commonly three areas of compression;
1. the border of the 1st rib and the anterior and medial scalene muscles.
2. the middle of the clavicle (collar bone), 1st rib and upper scapula (shoulder blade).
3. under the Pec Minor tendon and coracoid process.
How did I get Thoracic Outlet Syndrome?
You may be more at risk of TOS if you have…
o an extra rib in the neck
o a previous injury in this area (clavicle or upper ribs)
o poor posture
o poor shoulder motor control
o are between the ages 30-50’s
o 4x more frequent in females
What signs and symptoms might indicate TOS?
These may differ depending on whether it’s the artery or veins involved…
Arterial
- Pins and needles, numbness, tingling or weakness in the shoulder, arm or hand.
- Pain with lengthening the arm (nerve)
- Sensation of arm heaviness, cold or loss of colour
- Reduced radial pulse strength
Venous
- Swelling
- Reddened and/or warm skin
- Raised veins
Can physiotherapy help?
A physiotherapy assessment is crucial in negating all other possible diagnoses and assists treatment, management and onward referral if necessary. Thoracic Outlet Syndrome is very rare so ruling in or out any other likely causes of your pain is critical.
Conservative management should always be trialled initially to reduce symptoms and improve function and return to work before considering if further imaging may be required and/or if a combination of allied health professionals will be required to assist with overall management.
PREHAB: TAKING CONTROL OF YOUR RECOVERY
Optimising recovery from surgery:
Regardless of what it’s for, surgery can be scary and overwhelming. It is normal to feel a sense of helplessness or feeling as if you don’t have control over the end outcome. However, it is important to understand that you play the single most important role in the outcome of your recovery and it starts long before you meet with your surgeon. Preparing your body and mind for what you are about to encounter is an important aspect of recovery and creates good habits for your post-surgery rehabilitation.
How do you do this, you ask?
We call this Prehab
Prehab is a programme designed to prevent injuries before they actually occur. This can be applied to anyone or any injury however in the context of surgery it is you taking an active approach to prepare yourself physically and mentally for what you are about to go through. It plays a massive part in giving you the power to control the success of your upcoming surgery.
Why should you do Prehab?
Numerous studies have shown that patients who participate in Prehab have significantly better outcomes than those who do not. Those who undergo prehab generally have quicker recovery times, return to sport faster, have less complications and are generally more satisfied with their end outcome.
Does this apply to me?
Prehab is highly recommended for anyone planning to undertake or has been referred for surgery. Research has shown Prehab to be effective in enhancing recovery for patients undergoing total hip and knee replacements, ACL reconstructions, shoulder surgery such as rotator cuff repairs and lower back surgery.
What does it involve and how long for?
Ideally, undergoing 6-12 weeks of Prehab prior to surgery will optimise post-surgical outcomes. In most situations this is not possible due to availability with your surgeon. This does not mean that Prehab won’t help be helpful for you. As they say, something is better than nothing and there are still many meaningful benefits to be gained with only 2 weeks of preparation.
5 reasons to Prehab:
1. Get control of your pain:
A prehab program should give you the tools to minimise pain. Reducing pain early will enable normal muscle activity and put you in a good head space leading up to surgery.
2. Get in optimal physical shape:
Through a specific exercise program, you can improve muscle strength, flexibility, balance and coordination which has shown to optimise and speed up the recovery process post-surgery. Additionally, improving general fitness and wellbeing has many added benefits such as weight loss and improving mental resilience which is extremely important to recovery.
3. Create good habits and kick the bad habits
Firstly, creating good habits beforehand will make your life so much easier once you have been discharged from hospital. Good habits start with getting in a healthy exercise regime This extends to healthy sleep, nutrition and lifestyle habits which your physiotherapist and health practitioners can guide you on.
Conversely, bad habits will have the opposite effect, so you can imagine the importance in changing these prior to surgery.
4. Manage anxiety/stress
It is completely normal to feel anxious or stressed prior to surgery. In addition to physically preparing yourself you must also get yourself in the right headspace. Prehab will help mentally prepare you by getting you in a good mindset for the upcoming rehabilitation process. It will also teach you appropriate coping strategies to deal with pain and stress associated with the injury.
5. Speed up your recovery and reduce post-operative complications
Prehab sets you up for a successful recovery leading to quicker recovery and return to sport times. It also reduces the risk of common complications associated with surgery.
Please feel free to contact our team at East Vic Park Physio on 9361 3777 if you have any questions or would like to find out if Prehab is appropriate for you.
AC Joint pain - The "Other" Shoulder Pain
Anatomy
The Acromioclavicular (AC) joint is located at the lateral tip of the shoulder. The joint is formed by two bones, the clavicle (collarbone) and the acromion (a portion of the scapula/shoulder blade). In between the joint sits a fibrocartilage meniscal disc and the bones are connected by a number of ligaments, muscles and a joint capsule.
Role
The AC joint acts as a pivot point in the shoulder allowing the shoulder blade to rotate as the arm is lifted upwards. If it is dysfunctional it affects the control of your shoulder.
About
The AC joint is very commonly injured in contact sports that involve tackling like rugby or AFL. This is classified as a traumatic injury in which the ligaments can be torn and the capsule disrupted which results in the bone separating. However, you can also have AC joint pain from overloading the joint or degeneration of the fibrocartilage meniscus. It can also develop into a condition called osteolysis which is quite common in gym goers.
Differentiation from “bursitis” or impingement (common shoulder pain)
Shoulder bursitis/impingement is a very common condition in which the bursa and tendons in the shoulder get inflamed or overloaded. Often a cortisone injection is prescribed which can reduce the pain if the bursa is the main issue. However, if it is not the correct diagnosis then ongoing pain and disability can perpetuate. It is very important to get your shoulder assessed by a physiotherapist to differentiate between the two conditions so the right treatment plan can be selected. Please note that Impingement CAN occur as a result of AC joint pain or injury but is not the primary diagnosis.
Common presentation
· Pain at the top or tip of the shoulder
· Difficulty lying on the shoulder
· Difficulty bringing the arm across the body
· Pain with lifting an object above your head
· Pain with gym activities like bench press
General advice
· Try icing the area especially when it is painful
· Rubbing voltaren gel on the area can help reduce pain, the joint is superficial enough for the gel to have some effect
· Applying taping to pull the shoulder upwards can take the pressure off the joint and relieve discomfort
· A structured rehab program is helpful in making the muscles around the joint stronger so there is less load on the area
· A cortisone injection can be helpful if conservative treatment isn’t effective, as long as they inject the right spot
· Most importantly, visit your highly trained physiotherapist for a thorough assessment and in-depth treatment plan
SPORTS INJURY MANAGEMENT SEMINAR
Whether your sports season is heading into finals or you are about to start gearing up for the summer season ahead, the information presented will help you to perform at your best.
a FREE seminar on sports injury management presented by the Physiotherapists at East Vic Park Physiotherapy. Topics will include muscle contusion (corkie) management, post-game recovery and a practical session on strapping.
Whether your sports season is heading into finals or you are about to start gearing up for the summer season ahead, the information presented will help you to perform at your best.
Appropriate for all athletes, parents, trainers and coaches.
Food will be provided - let us know if you have any dietary requests.
Spaces are limited so call us on 9361 3777 to secure your place now.