Whiplash Associated Disorders
Whiplash is a common term often related to motor vehicle accidents. But what exactly is whiplash? What is the best treatment and what does it mean for the longevity of your neck health? Read below!
Whiplash is a common term often related to motor vehicle accidents. But what exactly is whiplash? What is the best treatment and what does it mean for the longevity of your neck health? Read below!
What is whiplash?
Whiplash is otherwise known as an ‘acceleration/deceleration’ injury, where the head moves forwards and backwards at high speed resulting in a stretch to the structures in the neck. A very high velocity or complex accident can cause significant injury to these structures, however the majority of motor vehicle accidents DO NOT result in structural damage to the bones, nerves, joints or muscles of the neck.
Pain is often described as an ache in the neck, sometimes extending into the shoulders and arm, or up towards the head. Headaches and/or pins and needles may also present.
I have been in an accident, what should I do?
Stay calm – remember majority of car accidents do not result in significant damage to your neck. If you have been involved in an accident, it is best to book in with your GP as soon as possible. They will be able to rule out any serious injury, provide pain relief and refer you to begin rehabilitation. Once serious injury is ruled out, the best thing to do is keep your neck gently moving. Heat or ice packs may help to relieve pain and relax muscles.
What is the best treatment?
Hands on therapy is rarely used to treat neck pain after a motor vehicle accident. Research shows massage and manipulation do not show lasting benefit and in some cases can be quite uncomfortable. Exercise rehabilitation is the best treatment for neck pain following motor vehicle accidents, which may be a combination of stretching, range of motion, breathing and relaxation exercises and strengthening exercises. These exercises may be performed at home, in the gym or even in the pool depending on your ability. Your physiotherapist can guide you through a progressive rehabilitation program to get you back to your old self.
Will I always have neck pain?
Absolutely not! Once serious structural injury is ruled out, there is no reason why you can’t have a full recovery. Despite this, it is not uncommon for pain to last a long time after the incident, however the biggest predictors of poor prognosis and ongoing pain are catastrophising and lack of sleep. The type and speed of collision have very little effect on recovery time.
Dietary Supplementation
The dietary supplement and health food market is massive and is continuing to grow. To gain that extra edge it is not a surprise that athletes of all backgrounds find themselves drawn to additional dietary help to improve their physical output. Unfortunately, most of the supplements on shelves are not what they are made out to be and there is no substitute for good old-fashioned hard work.
The dietary supplement and health food market is massive and is continuing to grow. To gain that extra edge it is not a surprise that athletes of all backgrounds find themselves drawn to additional dietary help to improve their physical output. Unfortunately, most of the supplements on shelves are not what they are made out to be and there is no substitute for good old-fashioned hard work. However, it is not all bad news, there are some foods and supplements that have been backed by science that can play a marginal performance enhancing role in sport and exercise.
Here we will briefly go over some of these health foods and supplements that may have a positive effect on performance directly. There are also many other dietary foods/supplements that claim to have an indirect on performance such as aiding recovery, assisting muscle development or improving immune function which we will not go into detail.
Caffeine:
One of the most commonly used supplements and widely used legal drug (in the form of coffee). There is significant scientific for caffeine as a positive performance enhancement for some athletes in range of different types of activities.
Possible benefits are improved endurance capacity such as exercise time to fatigue and time-trial activities of varying duration (5-150min). This has been shown across activities such as cycling, running, rowing and various team-sports. Improvement in performance measures such as time-trial time have shown to range from 3-7%.
How does it work?
Caffeine is a stimulant which can enhance vigilance and alertness, perception of fatigue and exertion during exercise and improve neuromuscular function. It can also stimulate an endorphin release which can assist in feelings of wellness.
A systematic review by Ganio et al (2009) has shown 3-6mg/kg of body mass consumed 60 min prior to exercise is sufficient to provide positive effects. However lower doses <3mg/kg of body mass has shown to also be effective. To put that in perspective the average cup of coffee has about 100mg of caffeine in it.
Possible side effects:
Larger doses of caffeine have shown not to further increase performance enhancement and in fact increase likelihood of negative side effects.
Possible side effects include; nausea, anxiety, insomnia and restlessness. Caffeine is also a diuretic which can increase urine flow but is small when consumed at the doses that have shown to improve performance.
Sodium Bicarbonate:
Sodium bicarbonate is a commonly occurring substance in most foods. In fact, most households will have this In their kitchen without even knowing as it is commonly known as baking soda.
How does it work?
It helps regulate PH in the blood which commonly increases in acidity during exercise. Sodium bicarbonate is naturally occurring in the body and helps buffer excess acid that accumulates during bouts of high intensity exercise. By keeping muscle PH level closer to its normal it can enhance exercise capacity.
Sodium bicarbonate has shown to enhance performance during short term, high-intensity exercise of approximately 60s in duration of approximately 2%. Improvements reduce as duration of effort exceeds 10 min.
Protocol of use:
According to the evidence various strategies of consumption have been suggested.
1. Single dose of sodium bicarbonate of 0.2-0.4 g/kg of body mass, 60-150 mins prior to exercise
2. Split dosage (i.e multiple smaller doses totalling 0.2-0.4 g/kg) over 60-180 min
3. Serial loading with 3-4 smaller doses per day for 2-4 days consecutive prior to an event
Potential side effects:
It is well established that gastro-intestinal upset can be associated with sodium bicarbonate. Therefore, may not be appropriate for some athletes or ideal consumption strategies may be person dependant.
Creatine:
Creatine is naturally occurring substance in body where it is found in the substance creatine phosphate. Its use as a supplement has grown significantly over recent times. Creatine works by aiding resynthesis rate of the phosphocreatine energy system. In short aiding the use of the energy system in the body that is utilised in short, high-intensity bouts of exercise.
In term creatine has shown to have positive effects particularly in sports that involve repeated high-intensity exercise (eg. Most team sports). it has also shown to assist in increased gains of lean mass and muscle strength and power.
Potential side effects:
No negative health effects are noted with long-term use (up to 4 years) when appropriate consumption use is followed. However, a 1-2 kg of body mass increase has shown to be a possible side effect which is primarily the result of water retention. This is an important consideration as the possible detrimental effect of increase weight gain may outweigh the positive effect of creatine.
Nitrate or Beetroot Juice:
It may seem as an odd one to add in but nitrate which is readily found in beetroot has been shown to have positive performance enhancing benefits. High nitrate rich foods include leafy green and root vegetables, including spinach, rocket, celery and of course beetroot which accounts for one highest sources of nitrate.
How does it work?
Nitrate contributes to the production of nitric oxide in the body. Nitric oxide is a vasodilator which improves blood flow and oxygen delivery to muscles. It therefore can improve the muscle efficiency in utilising oxygen and can improve the performance and energy efficiency of type 2 or fast twitch muscle fibres.
Supplementation of nitrate has been associated with improvements of 4-25 % in time to exhaustion during exercise and 1-3 % in sport specific time trial events lasting less than 40 mins.
Protocol of use:
Nitrate consumption within 2-3 hours of activity as bee associated with improved performance. Prolonged use of nitrate also appears to be beneficial and has been suggested strategy for highly trained athletes where improvements from nitrate supplementation is smaller.
Potential side effects:
There appears to be few side effects or limitations to nitrate supplementation. It is suggested that there is potential of gastro-intestinal upset and therefore suggested to be trialled in trainings before the use in competition. It also appears that performance gains and harder to obtain in highly trained athletes.
Beta-Alanine:
A naturally occurring amino acid, beta-alanine plays a role in the development of a carnosine.
How does it work?
Similar to sodium bicarbonate, carnosine acts as a acidity buffer in the muscle and therefore helps maintain an optimal PH level for muscular performance. It helps resist muscle fatigue and in term potentially assists performance.
Protocol of use:
Beta-alanine is commonly found in meat, poultry and fish and therefore most people can get enough beta-alanine through their regular diet.
Dietary supplementation however can further assist our daily intake. It is suggested a daily consumption of 65mg/kg of body mass taken in 3-4 smaller doses throughout the day.
Potential side effects:
Possible side effects include skin rashes and/or transient paraesthesia (tingling feeling in the skin) when taken with high single doses. This effect is temporary and harmless.
It should also be noted the effectiveness of supplementation appears to be harder to realise in well-trained athletes.
It should go without saying please seek professional medical advice whenever considering whether additional dietary supplementation is right for you.
If must also be noted that inadvertently consuming a known banned/prohibited substance should be risk considered when weighing up the decision to pursue dietary supplementation. Please find some useful links below which can assist in determining whether a specific product is considered banned or has gone through the necessary batch testing to determine if it is safe for consumption under the anti-doping rules.
Useful resources:
https://www.informed-sport.com/
https://www.asada.gov.au/substances/check-your-substances
Common Adolescent Conditions – Part One: Ankle
This topic seems somewhat timely given these particular injuries are normally load related.
As discussed in my previous blog about Load Management, the last 6 months have played havoc with people’s Acute Chronic Workload Ratio and children/adolescents are no exception.
The conditions I will be discussing are usually related to a big spike in activity which has been the case this year with most sporting organisations eager to recommence their seasons. These spikes will be somewhat amplified in young athletes who participate in multiple sports or who are already specialising in their chosen sport which can mean numerous training sessions/games per week.
This topic seems somewhat timely given these particular injuries are normally load related.
As discussed in my previous blog about Load Management, the last 6 months have played havoc with people’s Acute Chronic Workload Ratio and children/adolescents are no exception.
The conditions I will be discussing are usually related to a big spike in activity which has been the case this year with most sporting organisations eager to recommence their seasons. These spikes will be somewhat amplified in young athletes who participate in multiple sports or who are already specialising in their chosen sport which can mean numerous training sessions/games per week.
Sever’s Disease
What?
An irritation of the insertion of the Achilles into the calcaneus. This differs from adult Achilles tendinopathy due to the immaturity of the adolescent skeleton which means it affects the actively remodelling trabecular metaphyseal bone.
How?
As mentioned previously, it is usually due to the area’s inability to deal with an increase in activity (particularly activity that uses that area eg running or jumping sports).
When?
More common in boys and usually between the ages of 10-15 compared with girls which is usually between the ages of 8-13.
How does it resolve?
Usually self resolves with time (6-24 months) however the reason it’s best to seek treatment/advice is due to the pain that accompanies the condition which can affect sports performance and most importantly day to day activities.
What is the treatment?
The main focus of treatment is to reduce pain levels. This can be done in a few different ways including:
- Manual therapy (eg muscle massage)
- Heel raises for footwear to offload the tendon
- Taping to offload the tendon
- Exercises to strengthen key areas
- Implementation of load management strategies (eg RPE scale)
- Advice regarding recovery (eg icing)
The main takeaways about the condition are:
- The adolescent will grow out of it
- It can still be quite painful however so there should be a focus on pain relief
- Load management with guidance from a physiotherapist can allow the continued participation in sport without compromising day to day function
If you would like your injury reviewed by one of our physiotherapists, then don’t hesitate to book an appointment. All of our physiotherapists specialise in sport and have had extensive experience with adolescent athletes.
Neck Pain and Upper Trapezius – The culprit or the victim?
Upper Trapezius gets a lot of blame as the cause of long-standing neck pain. If you have received treatment for ‘neck pain’ it may well have consisted of some massage, taping or advice to ‘relax’ your upper trapezius muscles - but is this what our treatment should target? Are we relaxing, stretching and massaging a muscle we should really be strengthening?
Upper Trapezius gets a lot of blame as the cause of long-standing neck pain. If you have been treated by a medical professional for neck pain you may well have received some massage, taping or advice to ‘relax’ your upper trapezius muscles - but is this what our treatment should target? Are we relaxing, stretching and massaging a muscle we should really be strengthening?
Are the upper traps overactive, or are they just weak?
In the presence of neck pain without precipitating trauma (i.e. pain following sustained or repetitive positions), most individuals will NOT have a specific pathoanatomical injury or source of symptoms.
Rather, pain seems to be the result of poor capacity or strength of the neck/shoulder complex, often with some dis-coordination of the muscles in this group.
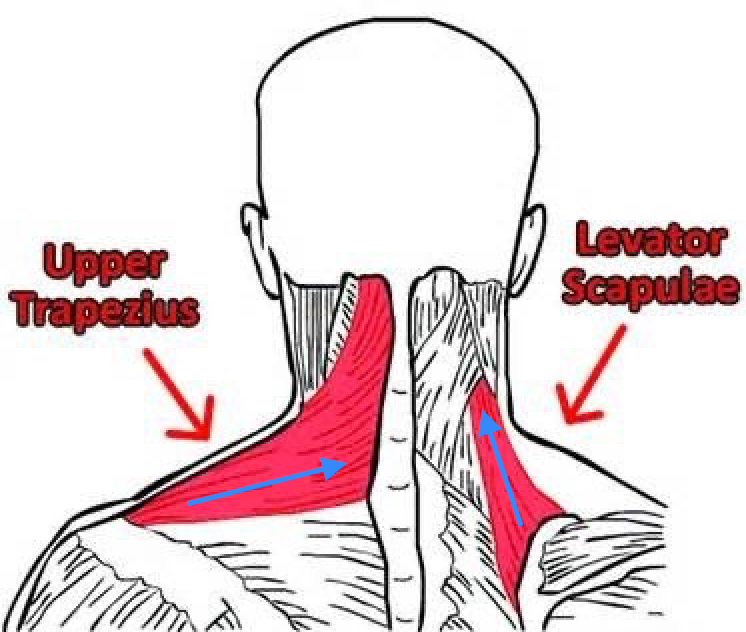
Patients commonly report their upper traps are ‘holding tension’ resulting in a shrugged type posture. If we look at the fibre orientation of upper trapezius, versus a lesser known muscle levator scapula, we can see that with our arms by our side levator scapula is at a more optimal position to elevate or shrug the shoulders.
In fact, upper trapezius does not show significant activation until late ranges of overhead movement. The shoulder complex is designed to elevate and by drawing our shoulders ‘down and back’ we are fighting against the natural biomechanical design of our bodies and potentially creating muscle discoordination.
Is a tight muscle an overactive muscle?
It is a common misconception tight or overactive muscles need to be massaged and relaxed. Often a muscle with increased tone or tension is due to that muscle being weak OR the entire muscular complex not working well together.
What does this mean for treatment of neck pain?
The last 10 or so years of research have shown increasing the strength of upper trapezius and muscles of the neck/shoulder complex reduce sustained and repetitively aggravated neck pain. A personal favourite of mine are lateral raises, working the upper trapezius in ranges of elevation where it is in the best position to active. A twice weekly workout of 3 sets of 8 repetitions have been shown to significantly reduce reported pain. General exercise such as walking, running or cycling should not be forgotten, especially if you are in a sedentary job.
This is also relevant for our gym population – your shoulder complex is actually stronger with some elevation. It is unnecessary and perhaps slowing your gains to ‘set’ your scapula in retraction prior to lifting.
Want more information on neck pain? Check out our past blog of the relationship (or lack thereof) between specific postures and pain.
PatelloFemoral Pain Syndrome (PFPS)
What is PFPS?
Patellofemoral pain is the most common cause of pain at the front of the knee.
It occurs with ‘patella mal-tracking’ i.e. when the under surface of the patella (kneecap) slides in the grove of the femur as the knee bends and straightens as the quadriceps contract and relax.
When the knee is bent, mal tracking often causes the patella to shift laterally, causing pain with squat, moving from sitting to standing and using stairs.
What is PFPS?
Patellofemoral pain is the most common cause of pain at the front of the knee.
It occurs with ‘patella mal-tracking’ i.e. when the under surface of the patella (kneecap) slides in the grove of the femur as the knee bends and straightens as the quadriceps contract and relax.
When the knee is bent, mal tracking often causes the patella to shift laterally, causing pain with squat, moving from sitting to standing and using stairs.
How did I get PFPS?
Causes of PFPS can vary, including;
o Over training i.e. people who over exercise with repetitive type movement i.e. cycling/hopping/jumping and running (especially hills and stairs) with insufficient time for recovery or excessive training loads.
o Change in training: i.e. changing footwear, running surface or increases in training intensity.
o Poor motor control at the quadriceps, hip (glutes) and foot/ankle (hyper or hypo-mobility).
o Abnormal knee/hip size and shape i.e. patella shape, femur shape or whether the patella sits high or low. Variations in an individual’s shape of the femur, tibia and/or hips can affect how the quadriceps muscles pull on the patella.
o Post-surgery i.e. post ACL surgery or after a lengthy time off
Where does it hurt?
Do you pain at the front of the knee around the kneecap? Is there pain AND clicking/crunching?
Note: A noisy knee without pain isn’t necessarily a bad thing.
Do I need a scan of my knee?
No.
In most cases this should be easily diagnosed by your physiotherapist or sports physician. If you aren’t getting results with your treatment and rehab then you may be referred for a scan.
What should I avoid doing?
- Complete rest
Repetitive running, cycling or deep squatting is likely contributing to your pain but engaging in physical activity is also helping to keep your muscles strong. Talk to your physio about activity modification.
- Don’t panic
Your knee will get better with targeted strength, stretching/rolling and other techniques. Note that due to the tissues involved, this can take months rather than weeks, persistence of your home exercise program will be important.
- Don’t train through high levels of pain, mild pain is usually ok.
Low or mild discomfort can be acceptable during activity, but if you are still sore 24-72 hours later then you may have done too much, too quickly.
- Exercises such as lunges and deep squats and stairs/hill running may aggravate your knee initially however you these will likely be re-introduced in the later stages of rehab.
I’ve been having physio and not getting better, what should I do?
Ask yourself;
- ‘Am I still over doing high impact activities, and/or underdoing strength / control activities?’
- ‘Am I getting enough recovery between sessions?’
PFPS frequently co-exists with other issues such as patella tendinopathy, fat pad impingement and patella hypermobility. It’s important to distinguish if any of these are involved by asking your physiotherapist.
Other less common diagnosis includes; bursitis, Osgood-Schlatter disease (OSD), Sinding-Larsen-Johansson syndrome and referred pain from the hip.
What’s the best treatment for PFPS?
Best practice for PFPS rehabilitation is a combination of…
- A short period of rest or de-loading
- Regular progressive loading
- Avoid painful knee ranges
- Taping and braces can help in the short term
- Your GP or health professional will be able to advise regarding anti-inflammatory use.
Speak to your physiotherapist who will assess and prescribe the optimum amount and intensity of exercises for you.
Author: Peter Gangemi - Master of Physiotherapy
Load Management
I started writing this blog about 2 months ago as Winter Sports pre-seasons started to ramp up. What a difference 2 months can make right? Back then, my purpose was to focus on the consequences of increasing physical activity (too much load) too quickly. However, on further reflection, the focus can also be on not enough physical activity (under-loading) which is probably more topical.
I started writing this blog about 2 months ago as Winter Sports pre-seasons started to ramp up. What a difference 2 months can make right? Back then, my purpose was to focus on the consequences of increasing physical activity (too much load) too quickly. However, on further reflection, the focus can also be on not enough physical activity (under-loading) which is probably more topical.
What is Load Management in sport?
Very basically it is the balance of physical activity and rest for an individual athlete.
This has two main purposes:
1. Reduce injury risk
2. Allow for Optimal Performance
From a physiotherapists perspective, we focus primarily on the first point whereas the coaching staff, club personnel and athletes are more involved with the second point. However, both groups work together to monitor an athletes load “ceiling” and “floor”.
What is the ceiling and the floor?
This refers to the max load an athlete can tolerate (the ceiling) and the minimum load an athlete should be maintaining (floor). Very basically, if you don’t continue to load your body, it’s capacity/resilience will drop which means it will tolerate less and less load over time (lower the ceiling). If an athlete then tries to increase their physical activity (eg pre-season) then they are at risk of overload injuries like stress fractures and tendinopathies. The ceiling is important because that informs the coaching staff of an athletes current limitations so they can plan for that in their trainings/gym sessions. Luckily, the ceiling can be increased with pre-planned and monitored loading over time. The main way this is monitored is through the Acute-Chronic Workload Ratio (ACWR).
What is the Acute-Chronic Workload Ratio?
Acute workload refers to the amount of loading over a week. Chronic workload refers to the average of loading over four weeks. Loading can be a number of factors eg kilometres per week which is applicable for marathon runner.
Optimal ratio is 1-1.25 so anything above or below can mean a large spike in injury risk.
Equation: (Acute workload) / (Chronic workload)
Eg week 1 40km, week 2 40km, week 3 50km, week 4 55km
So Acute workload is 55km (the latest week kms)
Chronic workload is average of four weeks ((40+40+50+55)/4) = 46.25
55/46.25= 1.2 (reduced injury risk)
As mentioned, ACWR can be built up over time. For example, the reason marathon runners can do 180km+ per week is because they have painstakingly built up their distance (and therefore ACWR) over years of training.
How to monitor relative load:
RPE Scale: Rate of perceived exertion times minutes per session
Smart watch that monitors distance, speed etc
GPS: electronic unit that calculates distance, speed, collisions etc
Subjective Questionnaires (eg Smartabase)
How is Load Management applicable to Elite Athletes?
You may see that every now and again an AFL player is ruled out of a game with “general soreness”, this is most likely because a players load is too high and they are at a high risk of injury so to reduce the risk, they won’t play the game. The same goes with NBA players (eg Kawhi Leonard in the 2018/2019 season) and high profile soccer players. Usually this is done during the season to make sure the player doesn’t get injured before the important part of the season (finals). It also serves to make sure they are “peaking” performance wise. The focus is on winning and the teams chances infinitely increases if their best players are;
A - able to play (no injuries)
B - optimally performing
How is it applicable to the everyday athlete?
Pretty much the same as above, just because they don’t get paid to play doesn’t mean they don’t want to perform well, remain injury free and win. However, it can be harder for everyday individuals to be able to monitor their loading as intensely as sporting clubs/elite athletes. So here are my top tips for monitoring loading if you don’t have a GPS etc:
Record each exercise session in terms of duration and RPE
Monitor your ACWR (as explained above) by reviewing and planning your training 4 weeks at a
time (at a minimum)
Keep an eye on types of physical activity and alternate if possible (eg running/jumping, weights, swimming, bike)
Apply the 10% rule: don’t increase distance, speed or weights more than 10% on your last session (especially if you can’t calculate your ACWR)
Lastly, listen to your body as it will most likely tell you when you need to “de-load”
Main points from this blog:
You need to load (even if you’re in isolation) otherwise you lose capacity
Load a bit more each week if you want to increase your capacity (not more than 10% is a good start)
Structure your physical activity to load manage which can reduce injury risk as well as improve performance
Listen to your body!
A big thanks to Glenn Stewart, Tim Gabbett and Lauren Shelley for all their work thus far in understanding load management.
If you would like some help load managing, make an appointment (call us on 9361 3777 or click the Book Now button) and any one of our highly trained physiotherapists will be able to assist you.
Workstation Ergonomics: Tips to staying pain free
With a large percentage of people now working from home the team at East Vic Park Physio thought it would be a good idea to provide some simple but useful information on workstation ergonomics.
Previous to what we used to think, there is not one way to correctly sit at your workstation. Your set up should be able to accommodate for a range of comfortable positions that you can frequently change throughout the day.
With a large percentage of people now working from home the team at East Vic Park Physio thought it would be a good idea to provide some simple but useful information on workstation ergonomics.
Previous to what we used to think, there is not one way to correctly sit at your workstation. Your set up should be able to accommodate for a range of comfortable positions that you can frequently change throughout the day. The optimal/most comfortable sitting position will change from person to person and will depend on:
The type of work being done
Visual demands
Individual body shape
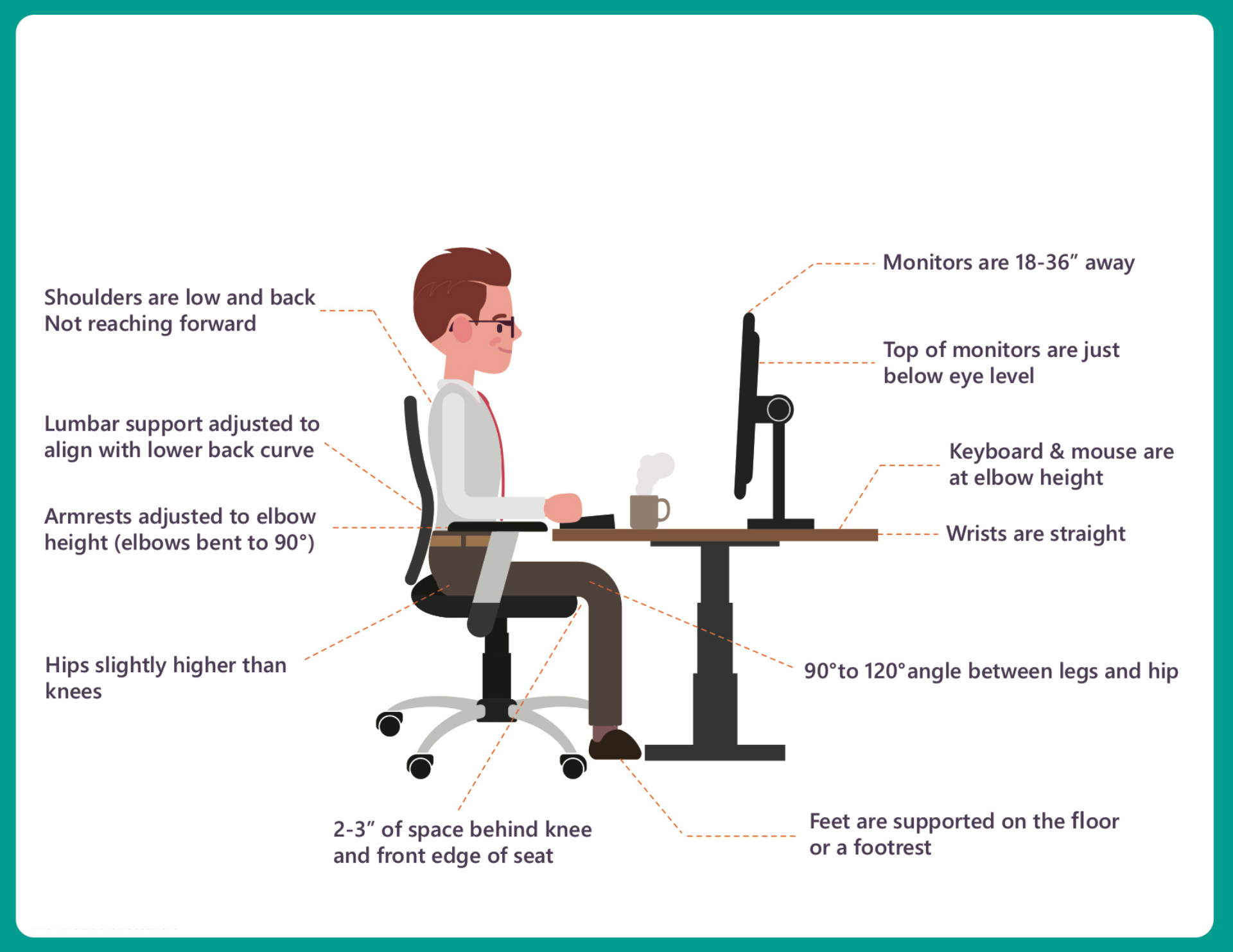
Figure 1: An example of an acceptable sitting position. It will allow for a range of supported postures that can be changed throughout the day.
Tips for setting up your home workstation:
Sitting with body close to desk
The head and neck are in a forward facing and in midline position (i.e no backward arching of the neck and or forward extension of the chin)
The shoulders are relaxed and relatively symmetrical, elbows close to the side of the body
The back is supported by the chair backrest. The curved lower part of the backrest should sit into the lower back
Having an open angle of 100-120 degrees (slightly more than right angles) at the hip. This can be achieved by adjusting the seat pan tilt and the backrest
o As a general rule have your knees at a height lower than your hip
Ensuring a gap or 2-3 fingers widths between the front of the chair and the back of your knees
Having feet flat on the floor or footrest
A Pain in the Neck: How does posture influence neck pain?
Neck or cervical pain is becoming increasingly common, with the highest prevalence among office and computer based workers. Physios commonly hear clients admitting to ‘bad posture’ – but do we really know what bad posture is?
Neck or cervical pain is becoming increasingly common, with the highest prevalence among office and computer based workers. Physios commonly hear clients admitting to ‘bad posture’ – but do we really know what bad posture is?
There can be many causes to neck or cervical pain, from a joint sprain, disc or nerve injury. This blog will focus on postural neck pain arising from a condition called myalgia, meaning tight, fatigued, painful muscles. This generally occurs without a history of trauma and yet is one of the most common causes of neck pain.
It is a common misconception that ‘sitting straight’ will solve all postural pain.
The neck is designed to move and although you may not realise, sitting in one position for an eight hour shift is quite a work out for your postural muscles.
Posture can have an influence on neck pain: rounded shoulders can create a forward head or chin poke posture, resulting in the muscles at the back of your neck working overtime to hold your head up. What some may not know is sitting very tall off the back of your chair can have an equally bad effect. An overly upright posture places a huge demand on the postural muscles, having a similar effect to clenching your fist for a long time – the muscles get tired and sore!
Although we aim for a ‘neutral’ posture, every body and spine is different and this ‘ideal’ posture looks different for everyone. The most important factor is finding a comfortable position, often with some low and mid back support. Having support over these areas helps ‘unclench the fist’ by offloading the postural muscles. It is important to remember that if you must be sedentary for a long period, you take breaks or change your sitting posture regularly. Neck stretches or rotations, walking to a collegue’s desk rather than emailing them or using a sit-stand desk are all ways to take a break from one sustained posture.
Studies have shown individuals with chronic neck pain (neck pain for 3 months or longer) show reduced endurance of deep stabalising muscles in the neck and have a reduced ability to maintain an upright posture. Although physiothearpists can provide hands on treatment to relieve symptoms, often the underlying cause of pain is a lack of strength and endurance of the muscles supporting the head. Manual therapy should always be paired with postural control and upper limb strengthening exercises.
Take home points:
Every spine is different, and there is not one ideal posture for everyone
Sitting in ANY posture for a prolonged time can cause pain, plus being sedentary isn’t good for our physical health
Finding a comfortable, supportive posture at work will reduce the risk of developing postural neck pain
General exercise and specific strength training for the postural muscles will increase robustness and significantly decrease the risk of neck pain
RECOVERY TIPS: WHAT DOES THE EVIDENCE SAY
In a world focused on optimal performance, adequate recovery is paramount in allowing consistent high intensity effort. Exercise in general uses various body energy systems in which the waste products (eg lactic acid) can hinder performance. The quicker the waste is processed and cleared out from the body, the quicker the body returns back to homeostasis.
In a world focused on optimal performance, adequate recovery is paramount in allowing consistent high intensity effort. Exercise in general uses various body energy systems in which the waste products (eg lactic acid) can hinder performance. The quicker the waste is processed and cleared out from the body, the quicker the body returns back to homeostasis.
The head of Discipline at the AIS, Shon L Halson, reviewed different recovery techniques in a published article that sought to determine the most effective methods.
Firstly, she identified the different factors affecting athletic performance which included:
- Environment (Temperature, altitude, humidity)
- Training/Competition (volume, intensity, duration)
- Health Status (Infection, illness, injury, muscle soreness)
- Psychological stress (Stress and anxiety)
- Lifestyle (Sleep, schedule, housing situation, leisure/social activities, relationships, job/school situation)
She then reviewed 6 methods that were thought to enhance recovery from the above factors and her findings are summarised in the table below:
She concluded that:
- Sleep conditions are very important
- Massage, 1-2 x per week can be helpful for elite athletes
- Contrast therapy should be 1 min hot, 1 min cold x 7 (cold temp 10-15 deg, hot 38-40 deg)
Here at East Vic Park Physiotherapy, we can provide advice on stretching, active recovery and hydro therapy programs as well as providing massage for recovery. Click on the BOOK NOW button on the top of the page or call us on 9361 3777.
Achilles Tendinopathy - What you need to know
With running season well upon us, here are some hints and tips about a common running injury achilles tendinopathy.
What is a tendinopathy?
Tendinopathy simply means that the tendon has failed to adapt to loading, doing “too much, too soon”.
Whether you have increased your load by volume, intensity or frequency… this amount was greater than the tendons capacity to cope and recover.
Load > Capacity
How did I get an Achilles Tendinopathy?
You may be more prone to a tendinopathy if you are a…
o Running / jumping / landing athlete i.e. distance running, basketball, AFL and netball.
o Weekend warrior who over exercises on weekends and under trains during the week.
o Older person with a history of poorly rehabilitated and/or grumbly tendon.
Where does it hurt?
Do you pinch your heel and feel your pain?
People tend to have a very specific site that is the source of their symptoms and can put their finger right on it.
Do I need a scan of my Achilles?
No.
In 90% of cases this should be easily diagnosed by your physiotherapist or sports physician. If you aren’t getting results with your treatment and rehab then you may be referred for a scan.
What should I avoid doing?
- Don’t rest
Staying off it completely will only increase the time it takes to rehabilitate the tendon.
- Don’t stretch/massage the tendon
Stretching and massaging the tendon won’t get it stronger. Muscle massage however, is ok. Stretch may feel good temporarily, however can make the tendon more irritable.
- Don’t train through high levels of pain
Low or mild discomfort can be ok during activity, but if you are still sore 24-72 hours later then you have done too much, too quickly.
I’ve been having physio and not getting better, what should I do?
Ask yourself;
- ‘Do I have the correct loading amount in my work out?’
… not too much or too little.
- ‘Am I sticking to the program?’
… over committing/loading or too many days between rehab sessions won’t help the tendon to strengthen and repair.
If you’re doing all these things right then discuss with your health practitioner where to go to next.
What’s the best treatment for Achilles Tendinopathy?
Best practice for tendon health is a combination of…
- Regular progressive loading, and
- Pain monitoring
- A short period of staying off the grumpy tendon may also be necessary.
- Your GP or health professional will be able to advise regarding anti-inflammatory use.
Speak to your physiotherapist who will assess and prescribe the optimum amount and intensity of exercises for you.
Author: Peter Gangemi - Master of Physiotherapy
Most Common Injuries in Martial Arts
Martial Arts will leave you black and blue but we love it and here you’ll read about the most common injuries we see amongst fighters including some input from Australia’s most decorated fighter and all round top bloke John Wayne Parr.
Most Common Injuries in Martial Arts
Being a martial artist has its pro’s and con’s and injuries are a major risk of the job. The following are some common injuries that fighters can expect whether training for fun and fitness or aiming to become the world champ.
1. Lacerations
The most common injury in the MMA and martial arts world. Australia’s most decorated Muay Thai fighter John Wayne Parr currently counts a total of 346* stitches from 146 professional fights (Muay thai and boxing).
General rules for whether you need stitches are;
- If the cut is greater than 1-inch in length or depth
- If you can see fat, muscle or bone
- Is the cut easily exposed to infection i.e. on the hand or fingers
- Difficulty with clotting i.e. prolonged bleeding >15mins
- Is it in a sensitive area i.e. the hands or face where reducing scarring is integral.
See your GP or present to your nearest emergency department if you fit any of the above categories.
Good luck JWP in your next fight against Anthony ‘The Man’ Mundine.
2. Cork / Contusion / Haematoma
Is an impact on the muscle with sudden, heavy compressive force i.e. opposition players knee. These can present either within a muscle (intra-muscular) or between muscles (inter-muscular).
Inter-muscular corks are sore to touch, can bleed down the limb i.e. thigh towards the knee.
Intra-muscular cork are also tender, and stiff to touch where stretching is difficult and movements like walking can be difficult without a limp. These can sometimes lead to solidification of blood within the muscle if not resolved, known as ‘myositis ossificans’.
Management;
- 0-48hrs: involves rest, ice, compression and elevation post game.
- 2-3days: see a physio/doctor for assessment and whether anti-inflammatories will be of use. Start some gentle stretching and movement i.e. exercise bike or light training.
- 3-4 days: gentle massage around cork and training as tolerated.
- 5 days: stretching and foam rolling around the sore spot and gentle heat packs may be useful.
3. Concussion – Knock Out aka ‘the Big Kaboosh’ aka ‘goodnight Irene’
The risk of concussion is significant in MMA due to high volume of punches, elbows, knees and kicks to the head. However, many fights are stopped due to submissions as opposed to head injury. In February 2019, the Australian Institute of Sport, Australian Medical Association and Sports Medicine Australia released a joint Position Statement on the management of confirmed concussions in athletes. (https://ama.com.au/position-statement/concussion-in-sport-2019 ). This states that athletes over the age of 18 should not return to contact activity sooner than 7-days, and 18-year-olds and under should refrain from risk of contact for 14 days or more and once cleared by a doctor with no signs of concussion still present.
A player should be immediately removed from the sport if any of the following occurred;
- Loss of consciousness
- A fall to ground without protection
- Seizure or tonic (rigid) posturing
- Impaired memory (date, location)
- Severe headache and other symptoms (below)
- Vomiting
- Deteriorating consciousness
- Vision loss/changes
- Non-typical behaviour
Signs of concussion may include;
- Loss of consciousness, headache, drowsiness or feeling like ‘in a fog’ or ‘slow’
- Dizziness or balance problems
- Confusion, sadness, irritability, nervous, anxiousness or emotional
- Blurred vision or sensitivity to light or noise
- Trouble sleeping
If any of the symptoms above are severe then the person should be taken directly to emergency and/or immediately be assessed by a doctor.
4. Fractures
a. Boxers Fracture
i. Occurs when a closed fist impacts with another hard object (head/floor) causing fracture at the head of the metacarpal (typically the 5th metacarpal).
ii. Signs: Swelling, redness, tenderness or crunching (crepitus) over the affected area.
iii. Diagnosis: Doctors or physiotherapist physical exam and X-Ray
iv. Treatment: Non-surgical cast and immobility or surgical pins and immobilisation cast.
v. Prognosis: up to 12 weeks
Others – can include any part of the body due to the high forces of usually bone on bone impact.
5. Cervical Disc Pathology – i.e. Neck cranks, rear-naked chokes.
Causes hyper flexion/extension or rotation to the neck. These often result in the fighter ‘tapping out’ prior to any serious damage. However multiple drilling, sparring and then fighting can place excessive stress on the neck discs, joints, ligaments and muscles.
Talk to your physiotherapist or GP immediately if you notice any of the following;
- Severe central neck pain
- Inability to move the neck >45° left or right
- Pins & needles, numbness or tingling into the arms and hands
- Severe shooting pains, electric shock or burning sensations in the arm and hands
- Strength loss in the upper limbs
Hot Tip: Learn your limits when training and ‘tap out’ early!
6. Dislocations / sub-luxations
The art of Brazilian Jiu Jitsu is designed to uncover the weakness at a joint and apply force so that the opponent taps before the trauma occurs. All dislocation/subluxations involve traumatic forces applied to a joint beyond its capability, leading to instability. Continuous micro-trauma may also lead to a joint becoming vulnerable over time.
A history of trauma puts you at increased risk of a repeat injury and continued clicking/locking/catching and instability indicates that the joint needs proper assessment and treatment. Never try to relocated a dislocated joint without a medical professional present.
Tip for young players… TAP EARLY
Author: Peter Gangemi - Master of Physiotherapy
Shoulder – Kimura / Americana
Shoulder – Kimura / Americana
Elbow – Arm bar
Thumb Dislocation
Busting Running Myths
Are you a seasoned runner or just starting out? Training for your first marathon or just enjoy your Sunday jog? Check out these commonly assumed running myths to know what is and isn’t important for improving performance and reducing injury!
Are you a seasoned runner or just starting out? Training for your first marathon or just enjoy your Sunday jog? Check out these commonly assumed running myths to know what is and isn’t important for improving performance and reducing injury!
Myth #1
‘The wrong shoe type can cause injury’
There is some largely subjective and unreliable evidence claiming barefoot running reduced injury by 2.6x compared to running in shoes
More recent research shows runners who change from a ‘bulkier’ shoe to a minimalistic shoe have a huge varied response in how their running style is affected from this change (with no correlation to injury)
There is a common belief that shoes should be fitted for a person’s foot type (i.e. pronated feet require more arch support). There is actually no evidence that this type of shoe ‘prescription’ affects performance or injury risk
Myth #2
‘Changing running style or becoming a forefoot runner is more efficient and reduces injury’
Forefoot strikers place more force through their ankles and calves, while rearfoot (heel) strikers place more force through their knees and hips
Despite the differing biomechanics, no running style has proved to enhance performance or reduce injury risk
There are large variations in the running styles of national 10K runners, with zero correlation to injury or finishing position
The biomechanical changes that occur when transitioning between running styles changes force distribution to certain muscles and joints, in fact INCREASING injury risk due to this shift in load
Forcing a running style that feels unnatural uses more energy when you run
Myth #3
‘Running will damage your knees’
Evidence is continuing to prove recreational runners are less likely to develop knee osteoarthritis (OA) than non-runners. It appears elite athletes who compete at an international level have the same risk of developing knee OA as non-runners.
Although further evidence is needed for a conclusive answer, a recent study has shown running does not speed the progression of existing OA and may even help to reduce symptoms.
There is strong evidence to suggest resistance training reduces the risk of OA, and slows progression of existing OA
Myth #4
‘You will get sore/injured if you don’t stretch’
Static stretching post run has no positive or negative influence on delayed onset muscle soreness, injury risk or running performance. That being said, as there are no detrimental effects and it can psychologically help runners ‘relax’ after a big training, stretching is still warranted if it feels beneficial for you.
It is well proven that sleep is one of the best forms of recovery. Athletes who sleep for less than 8 hours increase their injury risk by 1.7x compared to those getting 8 hours or more.
Re-fuelling your body with appropriate food will provide your cells with adequate nutrients to recover and grow muscle tissue. Low GI carbohydrates gives your body sustainable energy while you run, and High GI carbohydrates and protein are necessary for filling energy stores and muscle growth
An active warm-up including dynamic stretching (eg walking lunges, leg swings) and easy jogging is commonly used prior to exercise, but has not been proven to have an effect on injury risk.
Myth #5
‘The only thing that will improve running, is more running!’
The biggest injury predictor for runners is overload (doing too much too quickly). Total running load or volume should increase by no more than 10% per week to give your body time to recover and adapt.
Twice weekly strength training has been shown to improve performance, improve fitness or running efficiency and reduce injury risk.
There is no benefit to running performance by training low weight, high rep endurance exercises, nor circuit training.
Have a look at our ‘Basic Guide to Resistance Training’ blog for an explanation between different types of gym training
What does this all mean?
The number one biggest predictor of injury is a significant load increase of more than 10% per week (Running too much too quickly)
Choose a shoe you are comfortable in – there are more effective strategies to help your running than changing shoes
The body is adaptable and resilient, and there is no ‘perfect’ running style
Well thought out recovery (diet, sleep) is one of the most effective ways of reducing injury
Twice weekly strength training will reduce your injury risk and improve your running performance.
Our physiotherapists at East Vic Park Physiotherapy can answer all your running questions and can help review your running program to get you the best possible results
A QUICK GUIDE TO RESISTANCE TRAINING
Entering a gym can be a daunting task with people’s main complaint being that they don’t feel confident in using the equipment in terms of what weight to use, how reps, how many sets etc. From a physiotherapists perspective, avoiding exercise is not very beneficial for injury rehabilitation or prevention (or performance enhancement)! Here is a quick rundown on the general principles of gym training.
Entering a gym can be a daunting task with people’s main complaint being that they don’t feel confident in using the equipment ( eg. what weight to use, how many reps, how many sets etc). From a physiotherapists perspective, avoiding exercise is not very beneficial for injury rehabilitation or prevention (or performance enhancement)! Below is a quick rundown about the different types of parameters for resistance training and the meaning behind them.
Very basically, the four main prescriptions of resistance training are:
1. Power
2. Strength
3. Hypertrophy
4. Endurance
Each category has different parameters in terms of recommended weight, reps and sets (See Table below).
What is % of 1RM?
1 RM relates to the maximum amount of weight you could move with one repetition of an exercise. Percentage of 1 RM is then calculated and prescribed depending on the above table. There are specific ways to test 1RM but it must be done in a controlled environment with at least two people to help you with the weights.
1. Power (Exerting maximal force in as short a time as possible)
Characterised by low repetitions and sets, high weight and quick movement speed.
2. Strength (Ability to carry out work against a resistance)
Characterised by lower repetitions and sets, higher weight and normal movement speed.
3. Hypertrophy (Growth and increase of the size of muscle cells)
Characterised by medium repetitions, low sets and medium weight.
4. Endurance (Ability to work over an extended period of time)
Characterised by high repetitions and sets and low weight.
Rest times
2-3 minutes is recommended for most of the above categories especially for power and strength which utilises heavier weight. The muscles need time to replenish their energy source to be able to perform the required repetitions in the next set.
Safety
When lifting heavier weights or doing an exercise for the first time, it is best to have someone with you who is experienced. Most gym goers will have a “spotter” when they lift heavier weights. A “spotter” is there to assist you with handling the weights especially during the exercise where fatigue might mean you can’t complete the repetition.
What to choose?
Some people think that each of the above categories are discrete however there is good evidence that following your “strength” parameters will also result in an improvement in power and hypertrophy. The choice of category might come down to a person’s specific goals Eg. body builders might select hypertrophy as a focus. Keep in mind the World Health Organisation’s exercise recommendations for a healthy adult include two strength training sessions per week.
During an exercise rehabilitation program post injury, your physiotherapist should help to guide you with your program in terms of exercise selection. Usually there is a blend of all of the above categories at different stages of the recovery.
Here at East Vic Park Physiotherapy, all of our physiotherapists have had extra experience in strength and conditioning including coaching and our clinic is equipped with a gym so book in today to get a program sorted. Click on the BOOK NOW button on the top of the page or call us on 9361 3777.
Sleep Hygiene: Simple tips to keep it clean
here is a reason we spend approximately one third of our lives sleeping. It is a very important aspect of life and affects just about every biological system of the human body in one way or another. With that in mind it is still amazing how many people still deprive themselves of it. According to the Geneva Convention, sleep deprivation can be interpreted as a form of torture. So, it begs the question, why do we knowingly do it to ourselves?
There is a reason we spend approximately one third of our lives sleeping. It is a very important aspect of life and affects just about every biological system of the human body in one way or another. With that in mind it is still amazing how many people still deprive themselves of it. According to the Geneva Convention, sleep deprivation can be interpreted as a form of torture. So, it begs the question, why do we knowingly do it to ourselves?
It has been reported that up to 45 % of Australians suffer from inadequate sleep. With 24/7 nature of life today, the time we would normally allocate to sleep is now taken up with other “more important” activities such as studying for an exam, working late to earn that promotion or just partying. As a consequence, both sleep quality and quantity are being affected which is having a bigger impact than we think on our health.
Loss of sleep affects our ability to function at optimal efficiency. It can affect physical performance such as reaction time, tissue recovery and aerobic endurance as well as cognitive performance such as alertness and ability to perform complex problem-solving tasks.
In addition to the obvious and more noticeable and immediate side effects of sleep deprivation. There are many invisible yet serious consequences that affect our immune, hormone and metabolic function. They can subsequently increase the risk of obesity, diabetes, hypertension, depression, chronic pain disorders, developing the cold/flu and even increase the risk of sustaining sporting injuries by nearly 2-fold.
So how much sleep do i need?
Age and genetics play a key role in this. However generally:
· Infants need around 16-18 hours of sleep
· Teenagers need around 9 hours
· Adults need between 7-8 hours
Research has shown that both deprivation of sleep quantity and continuous sleep interruption (waking throughout the night) may have very similar effects. Therefore, not only getting an adequate amount of sleep is important but also sleep without regular waking is required for good sleep health.
Can I nap during the day?
Having an afternoon nap can help offset the negative effects of sleep deprivation. Research have also shown It can also have a positive effect on sporting performance although only for people who have had reduced night time sleep. Napping can be an effective way to improve sleep health. Just be mindful not to nap too late in the afternoon or for too long which may impact the quality of night time sleep. Napping/sleeping more than 30 minutes can lead to “sleep inertia” which is a physiological state where you feel less alert and drowsier when waking.
How can I achieve good sleep hygiene?
Good sleep environment
Numerous studies have shown a relaxing environment has a significant impact on sleep. A dark and quiet bedroom will help optimise sleep. Additionally, the temperature of the room can also play a big role with research showing a bedroom temperature of 18-22 degrees appears to best for a good night’s sleep. If you are still struggling to reduce external stimuli, the use of earplugs and eye masks can be helpful.
Get off the grid and unplug before bed
Limit use of devices such as phones, tablets, laptops at least 1 hour before bed. The use of these devices will make it difficult to relax prior to bed due to an increase in brain activity. Blue light also has a suppressive effect on production of the hormone melatonin which assists the body in falling asleep. If you must use a device close to bed Night Shift setting on devices or applications that filter blue light are recommended.
Avoid stimulants too close to bedtime
Avoid taking stimulants such as caffeine (within 5-8 hours before bed) and alcohol before bed. Although alcohol may seem to assist in getting to sleep faster it can actually affect the quality of sleep throughout the night
Food and drink
Avoid large meals and large quantity of fluids immediately before going to sleep. This has shown to have a negative effect on sleep. Try to aim to eat approximately 2-4 hours prior to sleep.
Have a routine
Try to have a consistent night time routine before going to bed each day. Additionally, try going to bed and waking up at the same time each day. This consistency will help regulate your body clock allowing for better quality sleep
Get out and exercise
Regular exercise is an extremely effective way to help manage stress and ensure you are tired enough to get to sleep at the end of the day.
Additionally, exposure to natural light during the day can help normalise your body clock and hormone levels and in turn assist in good sleep health.
Wind down before sleep
Try to reduce any physical, emotional and cognitive stressors. Activities that increase physical or mental alertness will make it difficult for the body to switch off when it’s time to go bed. If you are the type to have an active mind before sleeping, techniques such as mindfulness/meditation and journaling has shown to help switch off a racing mind.
Compartment Syndrome: The muscle pain not to be missed!
Earlier this year, St Kilda football club’s caption, Jarryn Geary, sustained an innocuous quad corkie, which later developed into compartment syndrome requiring immediate emergency surgery. Compartment syndrome is a serious condition which can occur acutely or over time and often requires prompt medical attention. Do you know the signs and symptoms to look out for?
Compartment Syndrome is a condition where excessive pressure in a muscle compartment restricts blood supply to that muscle. Muscles are surrounded by fascial connective tissue, which has very poor elasticity. Excessive swelling in the fascial compartment results in compression of blood vessels, then resulting in a reduction of oxygen to that muscle.
Causes
Compartment Syndrome can occur acutely after a traumatic injury (eg fracture, contusion or surgery), or as the result of a blood clot. This is caused by ongoing swelling or bleeding entrapped in the muscle’s fascial casing, increasing pressure within the muscle compartment.
Occasionally compartment syndrome can have no apparent cause, and develops over weeks or months, triggered by vigorous exercise such as running or cycling. Symptoms of chronic compartment syndrome typically worsen throughout exercise and ease with rest.
Signs and Symptoms:
- Severe pain in the muscle
- Swelling or tightness
- Pale or waxy appearance of the skin (due to restricted blood supply)
- Pins and needles, burning or numbness
What do I do if I suspect compartment syndrome?
Get assessed as soon as possible by your physio or GP, particularly if you have a history of trauma to the area. Through careful assessment, your health professional will determine if compartment syndrome is likely, and will refer you on as necessary.
Acute compartment syndrome is considered a medical emergency and can be life threatening if not addressed promptly. Insufficient blood supply over a long period of time means the area is deprived of oxygen and can result in tissue and nerve necrosis (death).
Chronic compartment syndrome can be harder to diagnose, due to transient symptoms that ease with rest. A measurement of intracompartmental pressure can be used to determine the severity of swelling in the fascial compartment. A pressure higher than 30mmHg indicates excessive pressure in the compartment. A CT or MRI scan may be recommended to rule out other serious pathologies.
Treatment Options
Acute compartment syndrome is a medical emergency and a fasciotomy of the affected compartment must be performed immediately to prevent permanent tissue damage. This involves cutting the encasing fascia of the muscle to release pressure, decompress the blood vessels and restore blood flow to the area.
In chronic compartment syndrome, it is recommended trying conservative rehabilitation, firstly by reducing or ceasing physical exercise/activities that exacerbate symptoms. From there, a physiotherapist can assess your strength and biomechanics, to identify any factors that may influence the condition. A referral to a sports doctor may be appropriate to discuss medication options. If conservative rehabilitation fails, or if an individual would like to continue their sport at the same level of intensity, fasciotomy surgery needs to be considered.
Thoracic Outlet Syndrome - A different shoulder diagnosis
The ‘Thoracic Outlet’ describes the compression of nerves (brachial plexus), arteries and veins resulting in pain, and altered sensations in and around the neck, chest and shoulder area. This is a rare syndrome only affecting 8% of the population.
What is thoracic outlet syndrome (TOS)?
The ‘Thoracic Outlet’ describes the compression of nerves (brachial plexus), arteries and veins resulting in pain, and altered sensations in and around the neck, chest and shoulder area. This is a rare syndrome only affecting 8% of the population.
There are commonly three areas of compression;
1. the border of the 1st rib and the anterior and medial scalene muscles.
2. the middle of the clavicle (collar bone), 1st rib and upper scapula (shoulder blade).
3. under the Pec Minor tendon and coracoid process.
How did I get Thoracic Outlet Syndrome?
You may be more at risk of TOS if you have…
o an extra rib in the neck
o a previous injury in this area (clavicle or upper ribs)
o poor posture
o poor shoulder motor control
o are between the ages 30-50’s
o 4x more frequent in females
What signs and symptoms might indicate TOS?
These may differ depending on whether it’s the artery or veins involved…
Arterial
- Pins and needles, numbness, tingling or weakness in the shoulder, arm or hand.
- Pain with lengthening the arm (nerve)
- Sensation of arm heaviness, cold or loss of colour
- Reduced radial pulse strength
Venous
- Swelling
- Reddened and/or warm skin
- Raised veins
Can physiotherapy help?
A physiotherapy assessment is crucial in negating all other possible diagnoses and assists treatment, management and onward referral if necessary. Thoracic Outlet Syndrome is very rare so ruling in or out any other likely causes of your pain is critical.
Conservative management should always be trialled initially to reduce symptoms and improve function and return to work before considering if further imaging may be required and/or if a combination of allied health professionals will be required to assist with overall management.
Injury Prevention: Part ONE – Groin Injuries
Prevention of an injury can be difficult as injury occurrence is usually a multi-modal. Extensive research has gone into the development of programs designed to address contributing factors of certain common injuries. Two common injury sites in sport are; groin and hamstring and both have been the subject of research articles investigating the efficacy of specific exercise intervention on prevention of injuries to those areas.
Prevention is the best cure - Desiderius Erasmus
Prevention of an injury can be difficult as injury occurrence is usually multi-modal. Extensive research has gone into the development of programs designed to address contributing factors of common injuries. Two common injury sites in sport are; groin and hamstring and both have been the subject of research articles investigating the efficacy of specific exercise intervention on prevention of injury.
GROIN
Groin injuries are a common occurrence in change of direction sports like soccer, basketball (e.g Lebron James recent injury) and Australian rules football. With the highest paid player in soccer earning $111 million per year, you can see why prevention of these injuries becomes very important.
Haroy et al (2017) looked at the inclusion of the Copenhagen exercise in the FIFA 11+ program (used as a warm up for soccer players) on improving hip adduction strength.
The Copenhagen Adductor (CA) exercise is a partner exercise where the player lies on the side with one forearm as support on the floor and the other arm placed along the body. The upper leg is held at approximately hip height of the partner, who holds the leg with one arm supporting the ankle and the other supporting the knee (position A in figure 1). The player then raises the body from the field and the lower leg is adducted so that the feet touch each other and the body is in a straight line (position B in figure 1). The body is then lowered halfway to the ground while the foot of the lower leg is lowered so that it just touches the floor without using it for support. It is performed on both sides.
Figure 1 The Copenhagen Adduction exercise. A start/end-position. B mid-position.
The article found that the CA exercise delivered in the below protocol (figure 2) resulted in an increase in hip adduction strength and as this is a risk factor for groin injuries, should be included in the FIFA 11+ to try to reduce the incidences of these injuries.
Figure 2 The prescription parameters for the CA exercise.
The CA is a fairly safe and easy exercise to self- integrate into the pre-existing FIFA 11+ protocol. However, even with the diligent performance of the protocol, groin injuries can still occur. It is always best to be assessed by a physiotherapist to ascertain a correct diagnosis so you can receive the best treatment possible for your specific condition. Here at East Vic Park Physiotherapy, our physiotherapists are very experienced in assessing and treating groin pain. Additionally, if you would like to know more about the CA exercise or the FIFA 11+ program then click the link at the top of the webpage to book an appointment or call us on 9361 3777. Below is a quick link to review:
https://www.fifamedicinediploma.com/lessons/prevention-fifa-11/
FIVE questions you should ALWAYS ask your orthopaedic surgeon before making a decision on managemen
Orthopedic surgeons are indispensable members of the health profession and have a level of anatomical and biomechanical knowledge and a degree of experience that is rarely surpassed.
However, if you’ve ever been for a consultation with an orthopedic surgeon, you’ll know how fast the appointment passes. Many of our patients have reported being in-and-out without feeling like they’ve said more than 10 words.
Most consults will last 10-15 minutes and within this short space the surgeon has a certain “volume” of assessment to conduct and information they MUST deliver. It’s easy to see why they can occupy most of consultation to you leaving little opportunity for questions or express your opinion. When the opportunity finally arises, many patients are so bombarded with information that they forget the questions that had been circling in their head for days!
The surgeon is not to blame here as they are exceptionally busy individuals and with a huge demand on their limited time and wealth of knowledge and experience.
However, it makes it imperative that you use the time well and ask direct and concise questions to ensure you leave the session fully informed and able to make the decision that is best for you in your unique situation.
We decided to put together a list of questions that you should leave the consultation with the answers to. We’d recommend you print the 5 questions (and add any others you think of) and review them quickly before leaving the consultation to ensure you don’t leave with unaddressed concerns.
1. Is there any way that I can AVOID surgery and how would outcomes compare if I took this option?
ALWAYS ASK THIS QUESTION.
There is ALWAYS an alternative when it comes to surgery.
For example, considering a shoulder dislocation in a young male AFL player, a stabilisation surgery is highly recommended. Without surgery, this patient would have at least a 70% risk of the injury recurring. In contrast, with a Latarjet stabilisation he could expect as low as a 2.7% risk of recurrence.
However, you always have choices. You could try and be one of the 30% who survive non-operatively. Likewise some patients might have no desire to return to AFL and consider moving to a less “risky” sport such as triathlons where an operation is completely unnecessary. So even though we would recommend the stabilisation surgery in general, for 3 different people, they may choose 3 different options based on their own preferences.
To sum up, there is never a single option and you need to ask this question to have accurate information to allow you to weigh up the positives and negatives of all your options and make the right choice for you.
2. How long CAN it take to recover - worst case scenario? What will I feel/how painful will it be?
Yes, the problem/pathology may be fixed with surgery, but the soft tissue that is disrupted in the process will be painful and take some time to recover from. This obviously depends on the nature of the surgery but it will almost always be very painful initially.
Everyone asks how long it will take to recover. The surgeon will often tell you how long it usually takes based on average outcomes.
However, humans are complex and varied creatures, and so surgery is not like changing a part on a car.
For example, if a surgeon advises that you CAN start walking crutch-free at 7 days-post does not mean that you WILL. Some may be ready at 4 days, while some may take 14.
Many patients get disheartened because they’re running behind the timeline, or because a friend had the same procedure and was much better at this point. However, the timeline is based on the average recovery, and your friend may be an unusually high performer due to a whole host of factors such as severity of condition, genetics and specific surgical differences.
To manage these complex situations, it’s always a good option to ask the surgeon how long it CAN take and ask for the worst case scenario. It’s important to not catastrophize about this as it is an unlikely outcome, but knowing it can help prevent frustration when your’re running behind the average timeline. This also gives us a clear definition to differentiate between things are going slowly and things are going wrong.
3. Are there other ways to do this surgery? Why have we chosen this variation?
This question will get a bit technical and some may prefer not to worry about it, but there are many ways of surgically achieving your goal.
Clinical trials help provide us with some answers as to which way is the most likely to be effective, but also provide an insight as to what can go wrong.
For example, to revisit shoulder dislocations, there are two surgical approaches most commonly used: the Latarjet procedure or an arthroscopic bankart repart.
There is now a solid amount of research indicating a higher rate of return to sport and a lower rate of recurrence of dislocation with a Latarjet. However, it is also associated with a slightly higher risk of adverse effects, so the decision is not always cut-and-dry.
Similarly, with and ACL reconstruction, choice of graft (hamstring, quad, patellar etc), tunnel location, single or double bundle, nerve block used can all effect outcome. Many factors influence the surgeons decision, and they will undoubtedly offer the best solution in their opinion. While you do no need to have personal knowledge on any of the above, we think it’s a good idea to obtain this information and understand WHY they have made the decisions they have.
It’s a good idea to write this down too as the technical terms are usually hard to recall.
4. How many of these procedures do you perform a year?
There is a body of research regarding total knee replacement operations and ACL repairs that consistently associates higher yearly volume (how many a year the surgeon performs) with fewer infections, shorter procedure time, shorter hospital stays, lower rate of transfusion, and better outcomes in the long-term. Research on other procedures is less available, but it’s safe to extrapolate that experience matters, just like any other profession.
If the surgeon has a relatively low yearly volume, it doesn’t mean that they will do a bad job as they will have undergone may procedures in their training and education.
Likewise, certain procedures as less commonly performed (e.g. repair of a complex bone break) so a high yearly volume is not feasible.
In any case, it’s worth asking how often they perform the procedure. If they perform a low number annually (<10 on a common procedure such as TKR), you could consider politely inquire if they have colleagues that specialize in this procedure and perform it more often.
With something as serious as a surgical procedure, you are always entitled to a second opinion. A good surgeon will have the self-awareness to know when they are and are not the right person for the job. If they can confidently assure you they have the necessary skill-set and experience, then you leave the consult knowing you are in safe hands.
5. Always ask YOURSELF, do I understand the diagnosis and/or the proposed solution? Test this by trying to summarize the information to you surgeon before you leave.
It’s a simple place to finish but make sure you fully understand what your surgeon has told you in the first place as errors in communication are so common in this situation.
The true test of this comes when you go home and try the “family/friend test”. If you can explain your problem well to family/friends, then you probably took the information in effectively. However, if it makes perfect sense in your head at the time, but you struggle to explain it later then you may not have understood it as well as you thought.
To ensure you pass the” family/friends test’, I recommend people try and perform a summary at the end of their consult, e.g.:
“So, if I understand correctly, my problem is that……and the proposed solution would fix this by…….all going well I should expect……but it may take as long as……..”.
This way, your surgeon will be able to highlight and correct anything that got lost in translation on the first occasion.
Conclusion:
There you have it – five important questions you should always ask in a consultation with an orthopedic surgeon. Any situation that requires the consideration of surgery is bound to be complex so it’s imperative that you get all the information. These five questions will help keep you focused and ensure you get the information needed to make a fully-informed decision that is right for you and your set of circumstances
PREHAB: TAKING CONTROL OF YOUR RECOVERY
Optimising recovery from surgery:
Regardless of what it’s for, surgery can be scary and overwhelming. It is normal to feel a sense of helplessness or feeling as if you don’t have control over the end outcome. However, it is important to understand that you play the single most important role in the outcome of your recovery and it starts long before you meet with your surgeon. Preparing your body and mind for what you are about to encounter is an important aspect of recovery and creates good habits for your post-surgery rehabilitation.
How do you do this, you ask?
We call this Prehab
Prehab is a programme designed to prevent injuries before they actually occur. This can be applied to anyone or any injury however in the context of surgery it is you taking an active approach to prepare yourself physically and mentally for what you are about to go through. It plays a massive part in giving you the power to control the success of your upcoming surgery.
Why should you do Prehab?
Numerous studies have shown that patients who participate in Prehab have significantly better outcomes than those who do not. Those who undergo prehab generally have quicker recovery times, return to sport faster, have less complications and are generally more satisfied with their end outcome.
Does this apply to me?
Prehab is highly recommended for anyone planning to undertake or has been referred for surgery. Research has shown Prehab to be effective in enhancing recovery for patients undergoing total hip and knee replacements, ACL reconstructions, shoulder surgery such as rotator cuff repairs and lower back surgery.
What does it involve and how long for?
Ideally, undergoing 6-12 weeks of Prehab prior to surgery will optimise post-surgical outcomes. In most situations this is not possible due to availability with your surgeon. This does not mean that Prehab won’t help be helpful for you. As they say, something is better than nothing and there are still many meaningful benefits to be gained with only 2 weeks of preparation.
5 reasons to Prehab:
1. Get control of your pain:
A prehab program should give you the tools to minimise pain. Reducing pain early will enable normal muscle activity and put you in a good head space leading up to surgery.
2. Get in optimal physical shape:
Through a specific exercise program, you can improve muscle strength, flexibility, balance and coordination which has shown to optimise and speed up the recovery process post-surgery. Additionally, improving general fitness and wellbeing has many added benefits such as weight loss and improving mental resilience which is extremely important to recovery.
3. Create good habits and kick the bad habits
Firstly, creating good habits beforehand will make your life so much easier once you have been discharged from hospital. Good habits start with getting in a healthy exercise regime This extends to healthy sleep, nutrition and lifestyle habits which your physiotherapist and health practitioners can guide you on.
Conversely, bad habits will have the opposite effect, so you can imagine the importance in changing these prior to surgery.
4. Manage anxiety/stress
It is completely normal to feel anxious or stressed prior to surgery. In addition to physically preparing yourself you must also get yourself in the right headspace. Prehab will help mentally prepare you by getting you in a good mindset for the upcoming rehabilitation process. It will also teach you appropriate coping strategies to deal with pain and stress associated with the injury.
5. Speed up your recovery and reduce post-operative complications
Prehab sets you up for a successful recovery leading to quicker recovery and return to sport times. It also reduces the risk of common complications associated with surgery.
Please feel free to contact our team at East Vic Park Physio on 9361 3777 if you have any questions or would like to find out if Prehab is appropriate for you.
Tennis Elbow: Getting to Grips with the issue
About:
Tennis elbow is a very common term used to describe lateral elbow pain. However, people can experience the condition without having ever picked up a racquet. The most up to date term currently is lateral epicondylalgia (LE) with “algia” meaning pain. This reflects the general shift away from it being considered an inflammatory condition in which the tendons around the elbow are inflamed. Rather, it is thought that the tendons become overloaded and sensitisation of the area occurs causing a heightened pain response that in turn causes inhibition of the muscles in the forearm. Inhibition results in a decrease in muscle “strength” which means everyday tasks like lifting a kettle become harder and tend to overload the tendons further causing more pain which causes more inhibition etc. (a vicious cycle of pain).
Even though the area of pain is usually focused around the outside of the elbow, it is actually the tendons of the forearm and wrist muscles that are affected. They come from a common origin point which attaches to the lateral epicondyle of the humerus bone. The implications of these tendons/muscles being affected is that it is mainly wrist and hand movements (e.g. gripping and lifting) and not elbow movements that are most painful.
Usually tendon pain occurs either through an acute injury or abnormal loading of the tendon (e.g. awkward tennis swing or a repetitive task at work). However, LE can also occur with no specific trigger. Around 40% of people will experience some form of LE in their lifetime and it is most prevalent those aged from 35-54 years (Bisset & Vicenzino, 2015). Regardless of the cause, it can be treated successfully to return the sufferer to full function. This will usually involve a loading program for the tendons to gradually improve their capacity and to “re-strengthen” the muscles. Rest alone does not address the muscle weakness or drop in capacity and this results in prolonging the injury. Weakness around the shoulder blade and shoulder muscles also needs to be addressed as the elbow can be the point of compensation for those areas further up the chain.
Common presentation:
· Pain in the lateral elbow or into the forearm
· Pain with tasks like lifting and gripping
· Weakness with tasks like lifting and gripping
General advice:
· Ice over the painful area (usually lateral elbow)
· Massage the forearm muscles (NOT the lateral elbow)
· Avoid poking or prodding the painful area (feels good at the time but really tends to make it worse)
· Use of a brace or taping around the upper forearm
· Avoid aggravating activities
· See your physiotherapist for a gradual loading program
· See your physiotherapist for an upper limb strengthening program
It is always best to be assessed by a physiotherapist to ascertain a correct diagnosis so you can receive the best treatment possible for your specific condition. Here at East Vic Park Physiotherapy, our physiotherapists are very experienced in assessing and treating lateral elbow pain. Click the link at the top of the webpage to book an appointment or call us on 9361 3777.
References:
1. Physiotherapy management of lateral epicondylalgia. Bisset, L & Vicenzino, B. 2015. Journal of physiotherapy (61), 174-181.