Achilles Tendinopathy - What you need to know
With running season well upon us, here are some hints and tips about a common running injury achilles tendinopathy.
What is a tendinopathy?
Tendinopathy simply means that the tendon has failed to adapt to loading, doing “too much, too soon”.
Whether you have increased your load by volume, intensity or frequency… this amount was greater than the tendons capacity to cope and recover.
Load > Capacity
How did I get an Achilles Tendinopathy?
You may be more prone to a tendinopathy if you are a…
o Running / jumping / landing athlete i.e. distance running, basketball, AFL and netball.
o Weekend warrior who over exercises on weekends and under trains during the week.
o Older person with a history of poorly rehabilitated and/or grumbly tendon.
Where does it hurt?
Do you pinch your heel and feel your pain?
People tend to have a very specific site that is the source of their symptoms and can put their finger right on it.
Do I need a scan of my Achilles?
No.
In 90% of cases this should be easily diagnosed by your physiotherapist or sports physician. If you aren’t getting results with your treatment and rehab then you may be referred for a scan.
What should I avoid doing?
- Don’t rest
Staying off it completely will only increase the time it takes to rehabilitate the tendon.
- Don’t stretch/massage the tendon
Stretching and massaging the tendon won’t get it stronger. Muscle massage however, is ok. Stretch may feel good temporarily, however can make the tendon more irritable.
- Don’t train through high levels of pain
Low or mild discomfort can be ok during activity, but if you are still sore 24-72 hours later then you have done too much, too quickly.
I’ve been having physio and not getting better, what should I do?
Ask yourself;
- ‘Do I have the correct loading amount in my work out?’
… not too much or too little.
- ‘Am I sticking to the program?’
… over committing/loading or too many days between rehab sessions won’t help the tendon to strengthen and repair.
If you’re doing all these things right then discuss with your health practitioner where to go to next.
What’s the best treatment for Achilles Tendinopathy?
Best practice for tendon health is a combination of…
- Regular progressive loading, and
- Pain monitoring
- A short period of staying off the grumpy tendon may also be necessary.
- Your GP or health professional will be able to advise regarding anti-inflammatory use.
Speak to your physiotherapist who will assess and prescribe the optimum amount and intensity of exercises for you.
Author: Peter Gangemi - Master of Physiotherapy
Proximal (High) Hamstring tendinopathy – A Real Pain in the Bum
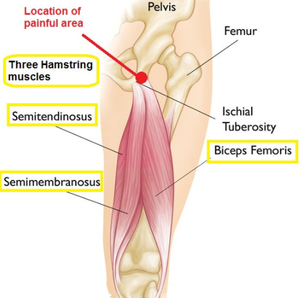
The hamstring consists of three muscles and it has a very important role in extending the hip from a bent position, e.g. initial phase of a deadlift, and in bending the knee, e.g. at the end of leg swing while running. While this muscle group is a very common source of problems, most commonly tearing when sprinting, this usually occurs in the middle of the muscle belly. In contrast, proximal hamstring tendinopathy refers to a reactive painful hamstring tendon at its attachment point on the base of the sit bone (ischium). This is why it is call a high hamstring tendinopathy.
Tendinopathy in the hamstrings is common in athletes, particularly in sports that involve large periods of time bent forwards, such as hockey, or involving high driving of the knees, such as sprinting or hurdling. However, it is often seen in other populations also., such as runners and even in the elderly.
How does it happen?
The hamstring tendon runs very close to the sit bone and is protected from compression and friction by the ischial bursa. If you gradually increase your training over time, these protective structures adapt providing greater protection. However, with sudden increases in the volume of compression on the tendon, this protection may not be sufficient, leading the tendon become extremely reactive and irritable. Sudden increases in compression can come from an increase in any of the following:
Direct compression from an external source, e.g. prolonged periods of sitting, especially on hard surfaces.
· Extreme positions of hip flexion pull the tendon tight against the sit bones, e.g. pulling knee close to chest, deep squats.
· Any hamstring stretch will likely compress the hamstring against the sit bone
· Contraction of the hamstring while already in a position of stretch will pull it tighter against the bone and increase the compressive forces, e.g. hurdling, sprinting (below)
Figure 1: Examples of positions of stretch with strong hamstring contractions that cause large volumes of compression of the hamstring tendon
It is important to again note that these compressive forces are normal for the hamstring. It is usually sudden changes in the volume of compression that is the problem, rather than compression itself.
The typical presentation is a deep ache or burning sensation right on their sit bone. It is usually quite focal but can sometimes radiate down the posterior thigh. Symptoms typically develop gradually over time, often without any clear moment of injury. They are usually worsened during activities involving hip flexion, hamstring stretch and hamstring contraction, particularly if all three are combined such as when lunging, squatting, sprinting, hurdling. Running up hills or stairs is usually worse than running down. Early on, the pain is usually worse at the beginning of activity, but warms up and gets better during activity, only to be very sore afterwards and the next morning. As it progresses and becomes more severe, it can worsen into activity and be quite painful even at rest.
What else could it be?
The anatomy in the area is complex and several other diagnoses should be clinically investigated and ruled unlikely before settling on a diagnosis of hamstring tendinopathy. The piriformis (circled in green) and deep gluteal muscles below it run close by and can develop tendon pain. The sciatic nerve (thick yellow band) also runs through this region and can become entrapped and irritated. Further, pain from the lumbar spine (lower back) and sacroiliac joint (where the pelvis meets the spine) commonly radiate into the buttock region and should always be screened for. In rarer cases, the shaft or the outside of the femur can impinge against the ischium causing irritation.
A comprehensive clinical assessment is usually sufficient to evaluate the likelihood of these various diagnoses and develop a comprehensive treatment strategy. In some cases, further imaging or referral to a specialist sports physician may be necessary.
How do I manage it?
1. Avoid compression – don’t stretch it!!
In the early stages, avoiding compression is the best way of settling symptoms in the early stages. Seating should be improvised or special cushions can be ordered to take pressure off the sit bones. Moreover, having a large glute bulk can provide extra protection. Static glute contractions can ease pain while sitting, and building glute bulk over time can be a useful strategy.
Avoid deep flexion exercises (such as squats or lunges), hamstring stretching and exercises that contract the hamstrings at long lengths such as stiff legged deadlifts or arabesques.
Later in rehab, once the tendon has settled down and is less irritable, then it is important to gradually add compressive activities back in to ensure full restoration of function. Your physio will again guide you through this process as it becomes appropriate.
2. Load management
For athletes, the hardest part is getting the balance right. This condition can be hard to manage if you continue to train at your usual level and you may be required to reduce or at least modify your workload. Typically, we are happy for our athletes to continue some volume of training with the condition so long as the pain is tolerable and doesn’t worsen from week to week. Use a consistent exercise performed at the same time every week to monitor weekly progress. If this is increasing, more modification may be necessary. However, if it is stable or decreasing than the current level is acceptable.
Activities such as sprinting, hockey, rowing, or uphill running are more provocative. We try to limit these activities to 2 times per week to allow sufficient recovery time between sessions. Outside of this, cross training is recommended to improve fitness without further irritating the hamstring tendon. We suggest aqua-jogging, swimming, cross-trainer, upright cycling with a well fitted seat height.
3. Hamstring strength exercises
Lower limb tendinopathies respond very well to exercise and we have found similar results in hamstring tendinopathies by strengthening the hamstring itself. The trick is to get the right exercise for the right person at the right time. The best way is to get a specific rehabilitation program from your physiotherapist. They can guide you on which exercise to do at each stage and how many sets/reps/frequencies to ensure you get the best-fit dosage for your condition at its specific stage.
4. Biomechanics
Certain characteristics may put someone at an increased risk of developing a hamstring tendinopathy. For example, having a very stiff lower back, or tight hip flexors will pull your hips into a forward tilt. This means that while running, your hamstrings will be on a higher stretch throughout. Addressing these biomechanical factors can be very useful in reducing symptoms during activities and preventing reoccurrence.
What else can I do?
· Dry Needling and Soft Tissue Mobilisation
A tendon that does not like compression is unlikely to respond positively to pressing on it or sticking needles in it. However, soft tissue work can provide effective pain-relief if directly at highly toned muscles surrounding the irritable tendon, such as the hamstring muscle belly, or deep gluteals. Likewise, soft tissue work may be useful to help address some of the biomechanical deficits mentioned above, such as releasing the lower back or hip flexors.
· Anti-inflammatories
Anti-inflammatories such as ibruprofen can be useful to settle the pain in hamstring tendinopathies, particularly if caught early and applied stringently over a short period. We would suggest visiting your physician before trying this approach. It is important to couple this approach with comprehensive rehabilitation to ensure full restoration of hamstring function and reduce the risk of reoccurrence.
· Injection
Corticosteroid may provide some short-term relief (approximately 6 weeks). However, symptoms tend to reoccur once the effects of the injection have worn off. Serial injecting is unwise as some evidence suggests it may cause deterioration of the quality of the tendon and worse outcomes. Corticosteroid should be used only with careful consideration after exhausting other management strategies.
PRP injections have been suggested to improve tissue healing. However, the currently available evidence does not support the use of this strategy, as it has a low likelihood of being any more successful than placebo.
· Shockwave therapy
Shockwave therapy has shown some promise, albeit with mixed results, in the treatment of lower limb tendinopathy. In our experience, it may lead to worsening of symptoms in irritable, acute tendinopathies. However, it can be a useful strategy in some patients, particularly those with more chronic and less irritable tendinopathies.
· Surgical management
Surgical procedures have been described but should be an absolute last resort for the management of hamstring tendinopathies and only used when all other strategies have failed.